About Ticks
- Tick Basics
- Tick Bites
- Geography
- Ticks & Rashes
- Tick Species & Diseases
- Tick Facts
- References
Tick Basics
Tick Basics
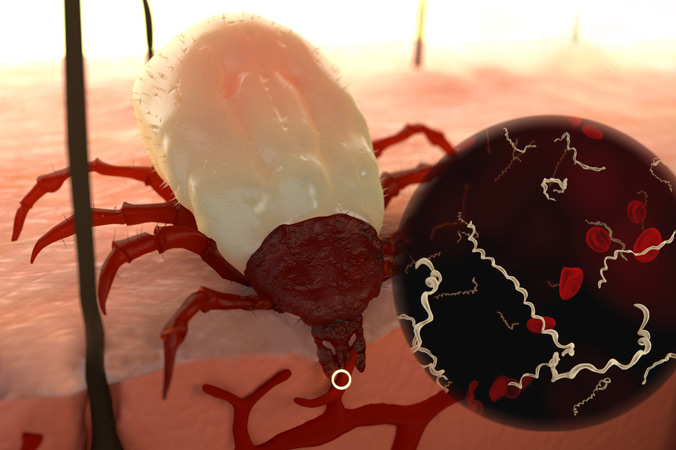
Ticks are tiny parasites that feed on the blood of their hosts (humans and animals) in order to survive and advance to the next life cycle stage. Most ticks have four stages: egg, larva, nymph and adult. The larva and nymph need a blood meal to move to the next stage. Ticks are extremely small, with the nymph the size of a pinhead. The female adult is much larger, and can grow to the size of a sesame seed.

From left to right: The blacklegged tick larva, nymph, adult female and adult male.
Not all ticks are alike, different species live in different regions of the country and can carry and transmit species-specific diseases. With one bite, ticks can infect a human with multiple pathogens, including the bacterium that causes Lyme disease. A single tick can carry over 40 other pathogens. [1] In the Westchester County, NY area, at least 25% of nymphs and 50% of female adult ticks are infected with the Lyme disease bacterium.[2]
Tick-borne infections that pose a threat to humans include Lyme disease, Ehrlichia, Babesia, Anaplasmosis, Bartonella, Rocky Mountain spotted fever, Borrelia lonestari, along with several other diseases that have recently surfaced.
Deer, birds and small rodents, like mice and chipmunks, are popular reservoirs for ticks.
Family pets can also carry ticks into the home and if loose on the animal’s fur, the tick can attach to an individual and become a potential threat.
Ticks typically live in tall grass, dense brush and wooded areas, and prefer shaded or moist spaces, like leaf piles. They can remain active in temperatures at or above freezing. In colder temperatures, ticks produce a sort of “antifreeze” that enables them to live through the winter months but they are not active.
Ticks do not fly, jump or fall from trees. Instead, they wait patiently for a host to pass by. Armed with sensors that detect carbon dioxide to identify mammals, ticks use their outstretched front legs to latch onto a host.
Tick Removal
Removing a tick as soon as possible is the best way to lower your chances of becoming infected with a tick-borne disease. To properly remove a tick, follow the steps below:
- Using tweezers (preferably with a pointed tip), grasp the tick close to the skin at a right angle.
- Pull upward with even pressure. Do not twist or pull quickly, since this can cause the mouthpart to break off and remain in the skin. (If this occurs, try to remove the mouthpart with tweezers. If unable to, leave it alone and allow the skin to heal. Without the body intact, the tick cannot transmit diseases.)
- Clean the area with rubbing alcohol, and wash hands thoroughly.
Do Not: Use a match to burn the tick off, or substances including petroleum jelly, or nail polish. These methods are not effective with removal.
(You may wish to save the tick by placing it in a ziplock bag in the freezer. Should you become ill and develop symptoms, the tick can be tested for diseases.)
Tick Bites
Tick Bites
Once attached, a tick embeds its mouthpart, called the hypostome, into the host and begins feeding. A tick’s saliva contains a mild painkiller, called kininases, which numbs the skin, so a person cannot feel the tick bite. As it’s feeding, an infected tick will transmit the pathogens directly into the host’s bloodstream. The bacteria travel quickly through the bloodstream and lymphatic system and can penetrate any tissues or organs in the body.
Once attached, a tick embeds its mouthpart, called the hypostome, into the host and begins feeding.
There’s been debate over how long a tick needs to be attached in order to transmit infectious bacteria. The CDC had been stating, “In most cases, the tick must be attached for 36 – 48 hours or more before the Lyme disease bacterium can be transmitted.” The CDC revised its statement saying, “Blacklegged ticks need to be attached for at least 24 hours before they can transmit Lyme disease.” One study found, the infection could be transmitted within 6 hours of a bite if the tick had been allowed to partially feed on an infected mouse.[3]
The risk of becoming infected increases the longer the tick is attached and feeding. However, physicians treating Lyme disease patients have found that diseases can be transmitted in less than 24 hours of a tick attachment.[4] Borrelia burgdorferi (Bb) has also been discovered in the salivary glands and ducts of ticks, which could explain a more rapid salivary transmission.[5-10]
Physicians should not rely on the presence of a tick attachment to consider Lyme or other tick-borne diseases in making a diagnosis. Studies have found that fewer than 40% of Lyme disease patients ever recall a tick bite.[11] A leading pediatric Lyme disease specialist, who has treated more than 15,000 children worldwide, has found that only 7% of his patients ever recall a tick attachment.
Often times, tick bites will be confused with spider bites. A tick bite can lead to chronic illness whereas a spider bite does not. Ticks can attach to any part of the body, but prefer areas where the skin is thin, such as behind the knees, belly button, groin, around the ears, and hairline. In small children, it is important to check their scalp carefully, since they’re closer to the ground.
Tick Geography and New Diseases
Tick Geography and New Diseases
The Northeastern states, Minnesota, Virginia and Wisconsin have the highest number of reported Lyme disease cases. People in other regions at risk go unreported. [12]
Some in the medical community argue that ticks carrying Lyme disease are geographically restricted to certain areas of the country. But others disagree. They claim that ticks have no boundaries, and changes in climate and a tick’s ability to travel long distances on a common host, like migratory birds are resulting in an increase and spreading of the tick population. For example, birds carry 50 million to 175 million I. scapularis ticks from the U.S. to Canada every spring.[13]
Additionally, new strains of Borrelia continue to emerge. According to a 2009 study, published in the Journal of Clinical Microbiology, Borrelia americana and Borrelia andersonii were found in the blood of symptomatic patients living in the Southeast. And, it was recently discovered that another tick species, the Lone Star tick, can transmit a Lyme-like disease, STARI Borreliosis.[14-16]
Newly discovered tick-borne diseases include:
- Borrelia miyamotoi, which is transmitted by Blacklegged or Deer ticks;
- Heartland virus, identified in patients in Missouri and Tennessee, is believed to be transmitted by Lone Star ticks; and
- Powassan virus, a potentially deadly virus transmitted by blacklegged or deer ticks.
Ticks and Rashes
Ticks and Rashes
The telltale sign of Lyme disease is the presence of the EM (erythema migrans) or bulls-eye rash. If it’s present, the diagnosis can quickly be made and treatment provided.

Fewer than 50% of Lyme disease patients ever recall seeing an EM rash.
However, in many cases, the EM rash does not appear or goes unnoticed. In fact, fewer than 50% of Lyme disease patients ever recall seeing an EM rash.[17]
Within 3 days of a tick bite, a red, itchy spot may develop but if it doesn’t expand larger than the size of a dime, this is merely an allergic reaction to the saliva and NOT the EM rash. The EM rash usually appears 3-30 days after the bite and may be circular or oval. The rash must be over 2 inches in diameter to be official. Note: The rash may present as over 2 inches without expanding.
The EM rash and other types of rashes can appear anywhere on the body. They do not always appear at the site of the bite. Some rashes can become very large. Other patients will have multiple rashes, which indicates that the Lyme bacterium has disseminated and spread to other parts of the body. The Lyme spirochete travel quickly through the bloodstream and lympathic system.
Rash Photos
Tick Species
Tick Species and Related Diseases
Blacklegged or Deer tick (Ixodes scapularis)
Lives: Northeast and Upper Midwest states
Transmits: Lyme disease, Ehrlichia, Babesia, Bartonella, Anaplasmosis
Note:
- Powassan disease is a newly discovered infection transmitted by the blacklegged tick.
- Borrelia miyamotoi infection is also new, and shares many similarities with Lyme disease.
- Ticks carry Bartonella. There is a dispute over whether the Bartonella infection can be transmitted by the bite of a tick or if a patient becomes infected through the mite of a cat, which also carries Bartonella.
Western Blacklegged tick (Ixodes pacificus)
Lives: Pacific Coast
Transmits: Lyme disease, Ehrlichia, Babesia, Bartonella, Anaplasmosis
American Dog tick (Dermacentor variabilis)
Lives: East Coast, some areas of Pacific Coast
Transmits: Rocky Mountain spotted fever, Tularemia, Ehrlichia
Note: It can be difficult to distinguish a blacklegged tick from the dog tick. The adult female deer tick can be nearly the same size as a dog tick. However, a deer tick typically has a black shield behind its mouthpart even when engorged, while the dog tick has a brown and white shield behind the mouthpart.
Brown Dog tick (Rhipicephalus sanguineus)
Lives: Throughout the United States
Transmits: Rocky Mountain spotted fever
Lone Star tick (Ambylomma americanum)
Lives: South-Central and Eastern states
Transmits: Tularemia, Ehrlichia, and Borrelia lonestari (STARI – Southern tick-associated rash illness), a disease similar to Lyme disease
Note: Nymph, adult male and female transmit diseases.
Pacific Coast tick (Dermacentor occidentalis)
Lives: Pacific Coast
Transmits: Rocky Mountain spotted fever, Tularemia
Rocky Mountain Wood tick (Dermacentor andersoni)
Lives: Rocky Mountain states
Transmits: Tularemia, Rocky Mountain spotted fever
Note: Adult male and female transmit diseases.
Disclaimer: New diseases carried by different tick species are emerging, and research continues into the role each species plays in transmitting such diseases. For example, 364D Rickettsiosis has been found in California and is transmitted by the Pacific Coast tick, and the Rocky Mountain Wood tick is known to transmit a virus, Colorado tick fever, according to the CDC.
If you have been bitten by a tick and are concerned about having been infected with a disease, contact a medical professional. If possible, remove the tick and save in a plastic bag in the freezer. Should you develop symptoms or become ill, the tick can be tested for diseases it may be carrying.
Tick Facts
Tick Facts
- Ticks do not jump, fly or fall out of trees.
- Ticks crawl up and prefer to feed in areas where the skin is thin (neck, ears, head region) and it’s easier to access blood. This makes it particularly dangerous for small children, who, because of their height, are closer to the ground and more prone to being bitten in that region.
- Ticks remain active in temperatures near or above freezing.
- You typically cannot feel a tick bite.
- Not all ticks carry diseases.
- Infected ticks can transmit multiple diseases with the same bite.
- You can only become infected with Lyme disease through the bite of a blacklegged or deer tick.
- Ticks only need to be attached for several hours in order to transmit a disease. However, the risk becomes greater the longer the tick is attached and feeding.
- Ticks do not need to be engorged in order to have transmitted a disease.
- Ticks crawling on a pet’s fur can be brought into the home and attach to a human.
- Ticks do not become embedded under the skin. The mouthpart only pierces the skin.
- Ticks like to hide in warm, hidden areas of the body (behind the knees, belly button, groin, under arms, behind the ears, neck and head region).
- Tick bites don’t always leave a rash. Less than 50% of patients ever report seeing the classic EM rash.
- A rash does not always appear at the site of the tick bite.
- Different types of rashes can appear. Multiple rashes can occur.
- Water (such as a shower or washer) will not kill a tick.
References
References
- Dumler JS, Madigan JE, Pusterla N, Bakken JS. Ehrlichioses in humans: epidemiology, clinical presentation, diagnosis, and treatment. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 45 Suppl 1, S45-51 (2007).
- Falco RC, Fish D. Prevalence of Ixodes dammini near the homes of Lyme disease patient in Westchester County, New York. Am J Epidemiol, 127(4), 826-830 (1988).
- Shih CM, Spielman A. Accelerated transmission of Lyme disease spirochetes by partially fed vector ticks. J Clin Microbiol, 31(11), 2878-2881 (1993).
- Hynote ED, Mervine PC, Stricker RB. Clinical evidence for rapid transmission of Lyme disease following a tickbite. Diagnostic microbiology and infectious disease, (2011).
- Benach JL, Coleman JL, Skinner RA, Bosler EM. Adult Ixodes dammini on rabbits: a hypothesis for the development and transmission of Borrelia burgdorferi. J Infect Dis, 155(6), 1300-1306 (1987).
- Ribeiro JM, Mather TN, Piesman J, Spielman A. Dissemination and salivary delivery of Lyme disease spirochetes in vector ticks (Acari: Ixodidae). J Med Entomol, 24(2), 201-205 (1987).
- Zung JL, Lewengrub S, Rudzinska MA, Spielman A, Telford SR, Piesman J. Fine structural evidence for the penetration of the Lyme disease spirochete Borrelia burgdorferi through the gut and salivary tissues of Ixodes dammini. Can J Zool 1989;67:1737–48 doi: 10.1139/z89-249.
- Lima CM, Zeidner NS, Beard CB et al. Differential infectivity of the Lyme disease spirochete Borrelia burgdorferi derived from Ixodes scapularis salivary glands and midgut. J Med Entomol, 42(3), 506-510 (2005).
- Piesman J. Dispersal of the Lyme disease spirochete Borrelia burgdorferi to salivary glands of feeding nymphal Ixodes scapularis (Acari: Ixodidae). J Med Entomol, 32(4), 519-521 (1995).
- Piesman J, Schneider BS, Zeidner NS. Use of quantitative PCR to measure density of Borrelia burgdorferi in the midgut and salivary glands of feeding tick vectors. J Clin Microbiol, 39(11), 4145-4148 (2001).
- Logigian EL, Kaplan RF, Steere AC. Chronic neurologic manifestations of Lyme disease. N Engl J Med, 323(21), 1438-1444 (1990).
- Bacon RM, Kugeler KJ, Mead PS. Surveillance for Lyme disease ─ United States, 1992-2006. MMWR Surveill Summ, 57(10), 1-9 (2008).
- Ogden NH, Lindsay LR, Hanincova K et al. Role of migratory birds in introduction and range expansion of Ixodes scapularis ticks and of Borrelia burgdorferi and Anaplasma phagocytophilum in Canada. Appl Environ Microbiol, 74(6), 1780-1790 (2008).
- Masters EJ, Grigery CN, Masters RW. STARI, or Masters disease: Lone Star tick-vectored Lyme-like illness. Infectious disease clinics of North America, 22(2), 361-376, viii (2008).
- Murdock JH, Yabsley MJ, Little SE et al. Distribution of antibodies reactive to Borrelia lonestari and Borrelia burgdorferi in white-tailed deer (Odocoileus virginianus) populations in the eastern United States. Vector Borne Zoonotic Dis, 9(6), 729-736 (2009).
- Diaz JH. Endemic tickborne infectious diseases in Louisiana and the Gulf South. J La State Med Soc, 161(6), 325-326, 328, 330-321 passim (2009).
- Krupp LB, Hyman LG, Grimson R et al. Study and treatment of post Lyme disease (STOP-LD): a randomized double masked clinical trial. Neurology, 60(12), 1923-1930 (2003).

What Is Lyme Disease?
Lyme disease is a bacterial infection typically transmitted through the bite of an infected tick. It is one of the fastest growing infectious diseases in the country, and the steadily increasing number of cases has led many in the medical/scientific community and legislative arena to deem the disease a “public health crisis” and “epidemic”. learn more →

Signs and Symptoms
Lyme disease has been associated with numerous neurologic, rheumatologic and psychiatric manifestations. However, the full range of symptoms needed to recognize the disease may not be apparent to a physician during a routine examination. learn more →

Role Of Co-Infections
Co-infections can be challenging to diagnose, as clinical features often overlap with many of the other tick-borne diseases, including Lyme disease. However, the importance of identifying and treating polymicrobial infections is critical in getting a patient well. learn more →












