Lyme Babesia co-infection is more common than many realize — and in some cases, it’s the Lyme that gets missed. In this case report, an elderly man diagnosed with Babesia almost had his Lyme disease overlooked. Only when he developed Bell’s palsy was the second infection identified.
The importance of clinicians considering other tick-borne diseases, such as Babesia, when evaluating patients with Lyme disease has been addressed in the literature. Surprisingly, however, physicians may actually not consider Borrelia burgdorferi (the Lyme pathogen) as a “co-infection” in patients diagnosed with a tick-borne disease.
Such was the case for an elderly man diagnosed with Babesia, who also had Lyme disease which was almost overlooked, according to a case report by Zaiem and colleagues.
Why Lyme Disease Gets Overlooked
The case report serves as a reminder to practitioners that as the number of reported cases of tick-transmitted diseases grows, Lyme disease should also be on their radar as a co-infection. For years, Lyme disease has been overlooked as a possible cause behind patients’ symptoms.
One study by Dr. Brian Fallon and colleagues found Lyme disease was overlooked an average of 2 years in patients who were later diagnosed with Lyme encephalopathy and a series of patients who were thought to suffer from a psychiatric illness. The undiagnosed Lyme patients with psychiatric illness were initially presumed to suffer from “paranoia, dementia, schizophrenia, bipolar disorder, panic attacks, major depression, anorexia nervosa, and obsessive-compulsive disorder.”
According to a case series by Dr. Daniel Cameron, there were Lyme disease patients whose illness was overlooked for years before they were diagnosed with and serologically confirmed with 5 out of 10 positive IgG western blot bands.
Treatment Delays Lead to Poor Outcomes
A delay in treatment can be concerning since it has been associated with poor outcomes for Lyme disease patients. For instance, Lyme encephalopathy patients, who were overlooked for an average of two years in the Fallon study, remained sick an average of 9 years after onset of illness.
Patients in the Cameron case series study, who experienced treatment delays, were 6 times more likely to fail their initial course of treatment than Lyme disease patients who were treated within 30 days of onset.
Case Report: Lyme Babesia Co-infection Almost Missed
“Co-infection with Borrelia should be considered in patients with atypical presentation or with a poor response to proper therapy,” concludes Zaiem.
A case report, published in QJM: An International Journal of Medicine, describes a 70-year-old man who presented to the emergency room with a 4-day history of headaches, high fevers, non-bilious vomiting and low urine output. Babesia was considered based on a 6-month history of living with his daughter in Eastern Long Island, NY. Malaria was also considered given he had emigrated from Bangladesh just 6 months prior to becoming ill.
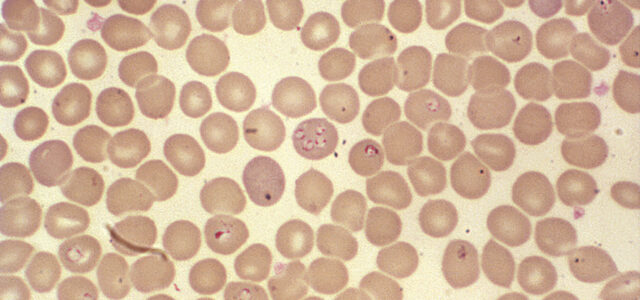
Laboratory tests supported the Babesia diagnosis. “Peripheral blood smear revealed intracellular ovoid rings resembling both Plasmodium sp. and B. microti rings,” states Zaiem. The PCR test came back positive for B. microti and the patient was started on a 7-day treatment with doxycycline and quinine to cover either infection. He showed improvement in both symptoms and laboratory findings.
Just prior to being discharged from the hospital, the man developed Bell’s palsy. He was tested and found to be positive for Bb and he was diagnosed with Lyme disease. The infection would have most likely been missed had the patient not developed Bell’s palsy — a symptom that only 9% of LD patients exhibited in the CDC’s surveillance database.
Lyme Babesia Co-infection Increases Severity
Illnesses transmitted by ticks can be complex. The importance in providing follow-up evaluations with patients treated for tick-borne diseases cannot be understated.
Given the growing number of studies finding ticks capable of harboring more than one disease-causing agent, Lyme disease needs to be considered in patients who have a documented tick-borne illness. A 2014 study found B. burgdorferi was detected in 55% of the ticks collected in an upstate New York region, followed by A. phagocytophilum (18.2%), B. microti (3.2%), and E. chaffeensis (1.5%).
Krause and colleagues described an increased illness severity if both Babesia and Lyme disease were present. Steere and colleagues reported patients with Lyme disease and Ehrlichia or Babesia tend to have more symptoms, in addition to fevers and chills, than patients who did not.
Co-infections Affect Treatment Outcome
An infection with more than one tick-borne infection can affect outcome. Krause concluded: “Physicians should consider use of tests designed to diagnose Babesiosis and HGE in patients with Lyme disease who experience a prolonged flu-like illness that fails to respond to appropriate antimicrobial therapy.”
Transverse myelitis and a fatal pancarditis are examples of poor outcomes in patients with both Lyme disease and Babesiosis.
Zaiem and colleagues remind clinicians: “When patients present with malaria-like illness in the areas endemic for Babesia infection, physicians should keep Babesiosis high on their differential list. Co-infection with Borrelia should be considered in patients with atypical presentation or with a poor response to proper therapy.”
References
- Zaiem F, Alkawam H, Lee S, Fabisevich M. Severe Symptomatic Babesiosis Co-infection with Lyme Disease. QJM. 2015.
- Fallon BA, Keilp JG, Corbera KM et al. A randomized, placebo-controlled trial of repeated IV antibiotic therapy for Lyme encephalopathy. Neurology. 2008;70(13):992-1003.
- Cameron DJ. Consequences of treatment delay in Lyme disease. J Eval Clin Pract. 2007;13(3):470-472.
- Krause PJ, Telford SR 3rd, Spielman A et al. Concurrent Lyme disease and babesiosis. Evidence for increased severity and duration of illness. JAMA. 1996;275(21):1657-1660.
- Aliota MT, Dupuis AP 2nd, Wilczek MP, Peters RJ, Ostfeld RS, Kramer LD. The prevalence of zoonotic tick-borne pathogens in Ixodes scapularis collected in the Hudson Valley, New York State. Vector Borne Zoonotic Dis. 2014;14(4):245-250.