Call for your appointment today 914-666-4665 | Mt. Kisco, New York
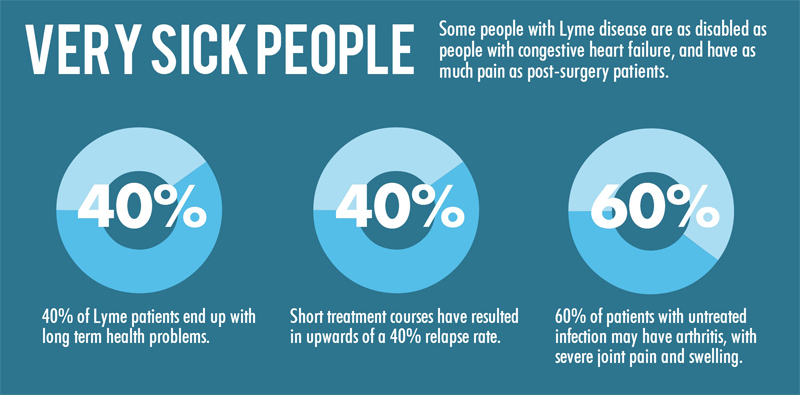
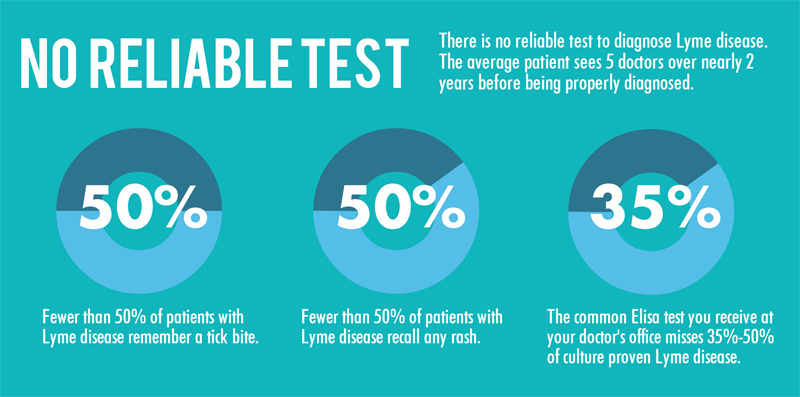
As these infographics on Lyme disease demonstrate, patients can suffer from long-lasting symptoms if not diagnosed early on and treated adequately. Diagnostic tests are unreliable. And contrary to popular belief, patients often don’t have the classic bulls-eye rash or recall a tick bite.
The data provided in these infographics are supported by peer-reviewed, published studies, as referenced below. (Infographic produced by Dr. Daniel Cameron & Associates)
40% of Lyme disease patients end up with long-term health problems
Thirty-four percent of a population-based, retrospective cohort study in Massachusetts were found to have arthritis or recurrent arthralgias, neurocognitive impairment, and neuropathy or myelopathy, an average of 6 years after treatment for Lyme disease. [1]
Sixty-two percent of a cohort of 215 consecutively treated Lyme disease patients in Westchester County, New York were found to have arthralgias, arthritis, and cardiac or neurologic involvement, with or without fatigue, an average of 3.2 years after treatment. [2]
At 6 months, 45% of patients reported neurocognitive difficulties, while 36% reported new-onset fatigue and 20% suffered from widespread pain. [3]
Short treatment courses have resulted in upwards of a 40% relapse rate
The following failure rates were taken from Table 5 of the ILADS evidence-based treatment guidelines. [4]
38.5% of patients failed treatment with 20 days of cefuroxime
33% of patients failed treatment with up to 19 days of doxycycline
22.8% of subjects failed treatment with up to 10 days of azithromycin
15.4% of subjects failed treatment with phenoxymethylpenicillin or amoxicillin
‘Success’ was defined as the complete resolution of an EM rash and all associated symptoms and findings, without evidence of disease relapse or the development of new manifestations consistent with Lyme disease during the observation period.
Subjects described by the investigators as ‘failures’ and those who were retreated (regardless of the post-retreatment outcome) were considered failures for the purpose of an outcome Intent-to-Treat (ITT) analysis.
Subjects who had ongoing symptoms at the final end point, including those described as ‘partial responders,’ were also considered failures. In some instances, this resulted in subjects being re-categorized as failures. Subjects who were ‘unevaluable,’ wrongly enrolled, non-compliant, withdrawn prematurely due to adverse reactions to their assigned antibiotic or lost to follow-up were also considered failures for the purpose of this analysis. [4]
60% of patients with untreated infection may have arthritis, with severe joint pain and swelling
Steere et al wrote a paper titled The Clinical Evolution of Lyme Arthritis states, “To determine the clinical evolution of Lyme arthritis, 55 patients who did not receive antibiotic therapy for erythema chronicum migrans were followed longitudinally for a mean duration of 6 years. [5]
The abstract states that from 4 days to 2 years after disease onset, more than 50% of subjects “had one episode or began to have intermittent attacks of frank arthritis, primarily in large joints; a few had polyarticular movement.” [5]
Fewer than 50% of patients with Lyme disease remember a tick bite
37% of chronic neurologic Lyme disease patients had a tick bite [6]
33% of Lyme encephalopathy patients had a tick bite [7]
Fewer than 50% of patients with Lyme disease recall any rash
25% of the first reported cases of Lyme disease had a rash [8]
39% of subjects had a rash in the Krupp NIH trials [9]
54% of subjects had an EM rash in the Fallon NIH trials [10]
The common ELISA test used at your doctor’s office misses 35-50% of culture proven Lyme disease
96 individuals in the study were diagnosed with Lyme disease. This was confirmed through the “gold-standard” culture test. Yet, only 37% of those 96 people actually tested positive on the ELISA. (The test most often used by physicians.) Therefore, the ELISA can miss 63% of Lyme disease cases. [11]
References
- Shadick NA, Phillips CB, Logigian EL et al. The long-term clinical outcomes of Lyme disease. A population-based retrospective cohort study. Ann Intern Med, 121(8), 560-567 (1994).
- Asch ES, Bujak DI, Weiss M, Peterson MG, Weinstein A. Lyme disease: an infectious and postinfectious syndrome. J Rheumatol, 21(3), 454-461 (1994).
- Aucott JN, Rebman AW, Crowder LA, Kortte KB. Post-treatment Lyme disease syndrome symptomatology and the impact on life functioning: is there something here? Qual Life Res, 22(1), 75-84 (2013).
- Cameron DJ, Johnson LB, Maloney EL. Evidence assessments and guideline recommendations in Lyme disease: the clinical management of known tick bites, erythema migrans rashes and persistent disease. Expert Rev Anti Infect Ther, 1-33 (2014).
- Steere AC, Schoen RT, Taylor E. The clinical evolution of Lyme arthritis. Ann Intern Med, 107(5), 725-731 (1987).
- Logigian EL, Kaplan RF, Steere AC. Chronic neurologic manifestations of Lyme disease. N Engl J Med, 323(21), 1438-1444 (1990).
- Logigian EL, Kaplan RF, Steere AC. Successful treatment of Lyme encephalopathy with intravenous ceftriaxone. J Infect Dis, 180(2), 377-383 (1999).
- Steere AC, Malawista SE, Snydman DR et al. Lyme arthritis: an epidemic of oligoarticular arthritis in children and adults in three connecticut communities. Arthritis Rheum, 20(1), 7-17 (1977).
- Krupp LB, Hyman LG, Grimson R et al. Study and treatment of post Lyme disease (STOP-LD): a randomized double masked clinical trial. Neurology, 60(12), 1923-1930 (2003).
- Fallon BA, Keilp JG, Corbera KM et al. A randomized, placebo-controlled trial of repeated IV antibiotic therapy for Lyme encephalopathy. Neurology, 70(13), 992-1003 (2008).
- Nowakowski J, Nadelman RB, Sell R et al. Long-term follow-up of patients with culture-confirmed Lyme disease. Am J Med, 115(2), 91-96 (2003).