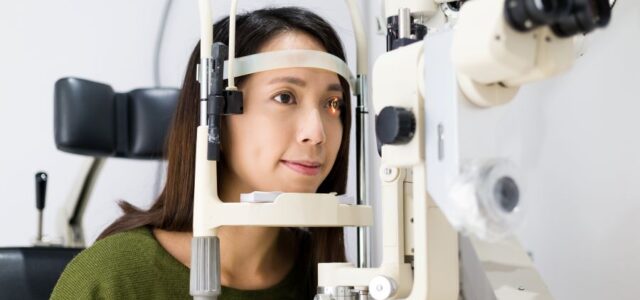
A 48-year-old woman with multiple sclerosis presented to her primary care physician with fever and sore throat. Three weeks later, she returned with photophobia, eye pressure sensation, blurry vision, pain with eye movements, and central scotoma.
A scotoma is a blurry or blind spot in the visual field while surrounding areas appear normal.
MRI and fundus exam confirmed the diagnosis of bilateral optic neuritis in Lyme disease.
Two months prior to her visit, the woman had removed a tick from her leg but did not report any rashes. Testing for Lyme disease was positive by Western blot.
Treatment and Recovery
The woman was hospitalized and treated with intravenous methylprednisolone (1g/day for 3 days) due to the degree of swelling, along with ceftriaxone (2g/day for 25 days) for Lyme disease.
One week after hospitalization, the patient reported her visual symptoms had resolved and she returned to her previous baseline.
Clinicians working in endemic areas should consider Lyme borreliosis in patients who present with bilateral optic nerve head swelling and painless progressive visual loss.
Systematic Review of Optic Neuritis Cases
Lu and colleagues reviewed the literature and found 11 patient cases of optic neuritis and Lyme disease. The authors collected cases demonstrating strong evidence of a causal relationship between Lyme borreliosis and optic neuritis to characterize the nature and clinical presentations.
The most common symptoms related to optic neuritis included:
- Blurry vision (11 cases)
- Headache (7 cases)
- Scotoma (3 cases)
- Painful ocular movement (3 cases)
Additional symptoms reported included:
- Neurological symptoms: paresthesia (3 cases) and ataxia (1 case)
- Arthralgia (3 cases)
- Nonspecific symptoms: fatigue, weakness, and myalgia (3 cases)
Clinical Presentation Differs from Typical Optic Neuritis
Only 2 of the 11 patients reported having an erythema migrans rash, while the majority did not recall a tick bite. Moderate vision loss was reported in 8 of the patients.
All patients responded well with combination corticosteroid and antibiotic therapy, or antibiotic therapy alone.
Typically, optic neuritis presents with acute, painful, and unilateral visual loss. However, in these Lyme disease patients, optic neuritis presented with bilateral optic nerve head swelling, painless visual loss, and moderate (better than 20/200) progressive vision decline.
This distinct presentation pattern can help clinicians recognize Lyme-associated optic neuritis.
Frequently Asked Questions
What is optic neuritis in Lyme disease?
Optic neuritis in Lyme disease is inflammation of the optic nerve caused by Borrelia burgdorferi infection. It typically presents with bilateral optic nerve swelling and painless vision loss, differing from typical optic neuritis.
How is optic neuritis from Lyme disease different from MS-related optic neuritis?
Lyme-associated optic neuritis typically presents as bilateral, painless, and progressive, while MS-related optic neuritis is usually unilateral, painful, and acute. However, patients with MS can also develop Lyme disease, complicating diagnosis.
What are the symptoms of optic neuritis in Lyme disease?
Common symptoms include blurry vision, headache, scotoma (blind spots), eye movement pain, photophobia, and progressive vision loss. Neurologic symptoms like paresthesia may also occur.
How is Lyme-associated optic neuritis treated?
Treatment typically includes intravenous antibiotics (such as ceftriaxone) for 2-4 weeks, sometimes combined with corticosteroids if significant swelling is present.
Do patients recover vision after treatment?
Yes. Most patients respond well to antibiotic therapy and experience significant or complete recovery of visual symptoms.
Clinical Takeaway
Optic neuritis in Lyme disease presents differently from typical optic neuritis, with bilateral involvement, painless progression, and moderate vision loss. In endemic areas, clinicians should consider Lyme disease in patients with bilateral optic nerve swelling, especially when combined with systemic symptoms or tick exposure history.
Related Reading
References
- Lu Y, Zand R. Characteristics of Lyme optic neuritis: a case report of Lyme associated bilateral optic neuritis and systematic review of the literature. BMC Neurol. 2022;22:113.

Scotoma, is this like a jelly spot on the eye that moves around causing the eyes to be blurry?
Calcification of pineal gland and lower aorta, are these seen in this Lyme/Babesia Disease?
Thank you for your response.
I have patients who I have had to refer to specialists to make sure I don’t miss another illness.