Call for your appointment today 914-666-4665 | Mt. Kisco, New York

Although Lyme disease is the most talked about tick-transmitted disease, Babesia is more common than you might think. In the 2015 issue of Trends in Parasitology, Diuk-Wasser and colleagues report that up to 40% of patients with Lyme disease experienced concurrent Babesiosis. [1]
This means that out of the estimated 300,000 cases of Lyme disease reported annually in the U.S., 120,000 of those individuals may also have Babesia. This is particularly alarming given that the disease can go undetected in asymptomatic individuals and is transmissible through blood transfusions or congenitally. Additionally, Babesia requires different treatment than Lyme disease.
The Babesia microti (B. microti) parasite that leads to Babesia is commonly seen in blacklegged deer ticks. But according to the authors, it’s also common to find ticks and enzootic hosts carrying both Borrelia burgdorferi (the causative agent of Lyme disease) and B. microti. In fact, between 12% and 42% of rodents are co-infected with both agents. This would suggest that “coinfection provides a survival advantage for both pathogens.” [1]
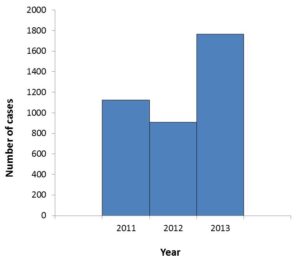
The first case of Babesiosis caused by the B. microti parasite was identified in 1969 in an individual who had vacationed in Massachusetts. It wasn’t until 2011, that it became a nationally notifiable disease with more than 1100 cases reported by the Centers for Disease Control and Prevention (CDC). Two years later, this number had risen to nearly 1800.
Setty and colleagues summarized their concern in a 2003 review, “Parasitemia in humans is transient and episodic. For this reason, there is a risk of asymptomatic donors transmitting the disease to recipients.” The authors raised concerns that there were 20 cases of Babesiosis and a variant Babesia strain called WA1 by red blood cells and blood component transfusions by 2003.
Babesia can lead to serious illness. Patients have presented with atrial fibrillation, [2] noncardiogenic pulmonary edema, [3] and anemia. [2] In New York, between 1982 and 1991, 7 people with Babesia died, while another patient on Nantucket Island developed pancarditis and died. [4]
Babesia occurs in individuals without the risk factors of increased age, prior splenectomy, immunosuppression, prematurity, and liver disease. [2] In one study of 192 patients, the average age was 46 years for individuals with Babesia. [5] The ages ranged from 27 to 83 years in a New York case series. [6] Five of 192 patients were immunosuppressed, [5] while none of the four subjects in another study had a splenectomy. [2]
Babesia can increase the severity of Lyme disease. Coinfected patients were more likely to have experienced fatigue, headache, sweats, chills, anorexia, emotional lability, nausea, conjunctivitis, and splenomegaly more frequently than those with Lyme disease alone. [7]
Babesia can also increase the duration of illness with Lyme disease. Babesia patients can remain symptomatic for years with constitutional, musculoskeletal, or neurological symptoms. One study found that 50% of coinfected patients were symptomatic for 3 months or longer, compared to only 4% of patients who had Lyme disease alone. [7] Meanwhile, one-third of patients with a history of both Babesia and Lyme disease remained symptomatic an average of 6 years. [2]
“The clinical pictures for 3 out of our 4 coinfected patients included a large number of symptoms, and 1 coinfected patient had persistent fatigue after treatment,” according to a study by Steere and colleagues. [8]
[bctt tweet=”Babesia and Lyme — it’s worse than you think” username=”DrDanielCameron”]
Babesia – difficult to diagnose
Equally worrisome is the fact that the disease can be difficult to diagnose based on symptoms. Nearly all patients with Babesia reported sweats. However, if the patient was coinfected with Lyme disease, the incidence of sweats dropped to 42%. Sweats can also be reported in other tick borne illnesses. [5]
 Babesia can also be difficult to diagnose with current testing. The parasite was detected microscopically in as few as one-third of patients with Babesia. [5] Specific amplifiable DNA and IgM antibody were more likely to be positive. [5] The reliability of tests for Babesia in actual practice remains to be determined.
Babesia can also be difficult to diagnose with current testing. The parasite was detected microscopically in as few as one-third of patients with Babesia. [5] Specific amplifiable DNA and IgM antibody were more likely to be positive. [5] The reliability of tests for Babesia in actual practice remains to be determined.
The Babesia tests can become negative. The Babesia sporozoites can be too few in number to be detected on a thin smear or can resolve with or without treatment. It’s been reported that a positive serologic test for B. microti will decay over time, leading to a negative test. Half of the patients with positive serologic tests for B. microti were negative on follow-up. [2]
Treating Babesia
Babesia cannot be treated with the same medications used to treat Lyme disease. Doxycycline is effective for Lyme disease, Ehrlichia, and Anaplasmosis but not for Babesia. Treatment with Mepron and Zithromax has been effective for Babesia. Quinine and clindamycin have also been effective but are associated with a higher rate of side effects. Flagyl and Tindamax drugs have been proposed but not well studied. The optimal treatment for Babesia has yet to be worked out.
Physicians have different views over the diagnosis and treatment of Babesia. The Infectious Diseases Society of America’s (IDSA) guidelines advise:
- Symptomatic patients whose serum contains antibody to Babesia but whose blood lacks identifiable Babesia parasites on smear or Babesia DNA by PCR should not receive treatment.
- Treatment is also not recommended for asymptomatic individuals, regardless of the results of serologic examination, blood smears, or PCR.
- Asymptomatic patients with positive Babesial smears and/or PCR should have these studies repeated, and a course of treatment should be considered if Parasitemia persists for >3 months. [9]
There are physicians who have elected not to treat Babesia patients, who are asymptomatic. In 1998, Krause and colleagues reported, “24 of 46 Babesia-infected subjects, who received no specific treatment, had Babesia DNA detectable in their blood for an average of 82 days.” [10]
In 2002, Krause et al reported, “Because symptoms had resolved or improved by the time concurrent Babesiosis or HGE was diagnosed, therapy was not administered to 38 (58%) of the patients with Lyme disease plus Babesiosis.” [5]
There are physicians concerned that symptoms of Babesia may be overlooked when evaluating patients. [11] The symptoms of chronic Lyme disease were overlooked for up to 14 years until reported in the 1990 New England Journal of Medicine by Logigian et al. [12] Meanwhile, the symptoms of Lyme disease were dismissed in by the IDSA Lyme disease guideline committee in 2000 and 2006 as nothing more than the aches and pains of daily living. [11] And the severity of the chronic manifestations were not validated until the 4 National Institutes of Health (NIH) sponsored clinical trials were completed. [13]
Sources:
- Diuk-Wasser MA, Vannier E, Krause PJ. Coinfection by Ixodes Tick-Borne Pathogens: Ecological, Epidemiological, and Clinical Consequences. Trends Parasitol, (2015).
- Wang TJ, Liang MH, Sangha O et al. Coexposure to Borrelia burgdorferi and Babesia microti does not worsen the long-term outcome of lyme disease. Clin Infect Dis, 31(5), 1149-1154 (2000).
- Golightly LM, Hirschhorn LR, Weller PF. Fever and headache in a splenectomized woman. Rev Infect Dis, 11(4), 629-637 (1989).
- Marcus LC, Steere AC, Duray PH, Anderson AE, Mahoney EB. Fatal pancarditis in a patient with coexistent Lyme disease and babesiosis. Demonstration of spirochetes in the myocardium. Ann Intern Med, 103(3), 374-376 (1985).
- Krause PJ, McKay K, Thompson CA et al. Disease-specific diagnosis of coinfecting tickborne zoonoses: babesiosis, human granulocytic ehrlichiosis, and Lyme disease. Clin Infect Dis, 34(9), 1184-1191 (2002).
- Meldrum SC, Birkhead GS, White DJ, Benach JL, Morse DL. Human babesiosis in New York State: an epidemiological description of 136 cases. Clin Infect Dis, 15(6), 1019-1023 (1992).
- Krause PJ, Feder HM, Jr. Lyme disease and babesiosis. Adv Pediatr Infect Dis, 9, 183-209 (1994).
- Steere AC, McHugh G, Suarez C, Hoitt J, Damle N, Sikand VK. Prospective study of coinfection in patients with erythema migrans. Clin Infect Dis, 36(8), 1078-1081 (2003).
- Wormser GP, Dattwyler RJ, Shapiro ED et al. The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis, 43(9), 1089-1134 (2006).
- Krause PJ, Spielman A, Telford SR, 3rd et al. Persistent parasitemia after acute babesiosis. N Engl J Med, 339(3), 160-165 (1998).
- Cameron DJ, Johnson LB, Maloney EL. Evidence assessments and guideline recommendations in Lyme disease: the clinical management of known tick bites, erythema migrans rashes and persistent disease. Expert Rev Anti Infect Ther, 1-33 (2014).
- Logigian EL, Kaplan RF, Steere AC. Chronic neurologic manifestations of Lyme disease. N Engl J Med, 323(21), 1438-1444 (1990).
- Cameron DJ. Clinical trials validate the severity of persistent Lyme disease symptoms. Med Hypotheses, 72, 153-156 (2008).

I am also interested in the correlation between elevated creatinine/BUN and kidney disease. My husband has been told that he has third stage kidney disease. We have had multiple tick bites (Hudson River Valley) and now wonder if babesia treatment might be indicated. No LLMD on board, unfortunately.
Kidney disease has been reported due to Lyme disease. I have not seen any literature addressing your question. Sorry
Does babesia effect labs such as creatine and general panel? White red count, etc…
Babesia may affect bloods the first week. Several tick borne illnesses appear to cause low white count.
thanks. I just have not seen it.
Creatine values are very high if you have damaged kidneys, caused by kidney infection or systemic infection. Babesia and Bartonella can cause quite serious kidney damage. The treatment goal is to kill the nasty pathogens in vivo, in this case Babesia, Bartonella, or both, using gram-negative, intracellular antibiotics.
I have not seen kidney failure due to Babesia in my practice. I am not in the ER for the first week to determine in there are cases of kidney failure.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8459803/
This article mentions kidney disease but not the blood levels.
My husband of 50 years old recently passed away from Babesia. He has a splenectomy when he was a child and by the time this illness was diagnosed, it was too late for him. His liver and kidneys shut down and the doctors treated him for alcohol withdrawal. I would love to see more awareness of babesia out there.
My husband had liver kidney failure as well, which I believe stemmed from Babesia (Positive FISH). His infectious disease doctors said the test was “invalid” but he responded to the Babesia treatment. Unfortunately it was too late and he went into full liver/kidney failure. He received a liver/kidney transplant in May 2017, but the liver is again showing signs of severe inflammation.
There are shortcomings of all tests including the western blot IgG and IgM patients. Doctors are often left withe clinical judgment when making a treatment decision if a tick borne illness is a possibility. It is also important to rule out other conditions.
My father was just recently diagnosed with Babesia. He is 78 years old and has no spleen. He is very ill and is having an allergic reaction to the Clyndamicin and Quinine. He can not keep any food or meds down. He is back in the hospital now and they started him on Azithromycin. There was a discussion early on about a “full body blood transfusion”. It seems to me this would be the best course of action given the circumstances, but his parasite level is only a level 3. Any advice would be greatly appreciated. Thank you.
I have used a combination of Mepron and Zithromax or Malarone with Zithromax on my patients. I am not convinced that Zithromax alone has value.
What was the treatment that was offered. Crazy question what about ivermectin? . Many doing as sr won’t help on dirt road discussions and facebook dort roads 2.0
I believe I was bitten over 20 years ago yet I don’t remember it. I was misdiagnosed with fibromyalgia, migraines and multiple psych disorders. I always felt they were missing something. I felt so sick and kept being told I was fine. I just found out I have Lyme Babesia and Bartonella. My regular doctors still don’t believe me but I have a positive clinical diagnosis and a positive iSpot lyme test. It literally explains everything I’ve gone through. I’ve been having scary chronic migraines that no medication will get rid of. I get complete loss of vision for a few seconds, vertigo, dizziness and aura along with swishing in my ears. Also the most awful pressure in my head and ears when standing or changing position. It feels like my pulse. My neck and shoulders hurt too but these are not tension headaches and my no is usually normal. Does this sound like something that could be explained by Lyme or Co Infections? All my Brain imaging has been normal.
You would be reasonable to include include a tick borne evaluation in your workup.
I was bitten by an insect on August 9, 2014 while lying in my bed. I broke out in hives, went to the ER and my heart just went off. I was hospitalized for 9 days on the cardiac floor. No one could tell me what was happening. Since then I have experienced pericarditis, tachycardia and since December, significant pain in my bones. I am desperate for answers. What is a tick borne evaluation?
Your doctor has likely already considered Lyme disease. You may benefit from being evaluated again for a tick borne infection by a doctor with experience in that area. You should also continue to look for answers with your cardiologist.
Alicia–where do you live? Have you investigated Chagas, or the cone nosed assassin beetle (kissing bug)? I have heard of severe reactions along these lines.
What is happening pls update ? Some have Mast cell histamine from food also from toxic over load? Can you share how your feeling and systems how your treating ?
Babesia and Bartonella are nasiter than Lyme disease for most. Babesia can take forever to get rid of sometimes it can take 9-15 months of intensive multi anti-malarial cocktails to eradicate this. A good check on whether you’ve gotten it under control is to check the inflammation of your liver and spleen. Babesia loves to hang out there (then again so does Bartonella). Forget getting tests they are quite inaccurate better off being treated based on symptoms.
The original study only prescribed 10 days of treatment for Babesia. The cases were caught at the time Babesia was in the red cell. The time to resolve Babesia that was not caught early is not as clear.
Hi dr Cameron . I came across this while researching symptoms . I am working with dr raxlen again . I had Lyme and co infections 19 years ago .I was misdiagnosed then for 3 years . I did get better : and then I 3 years ago o became so sick again after stress and a trauma . I was given phyc drugs for 2 years having to endure the most horrific pain . Coming off them. I was put into phyc hosputals and told it was in my head . I knew it was not . I been through this before . I had a test done by dr raxlen from vibrant lab . That showed possitive for Lyme b . Babesia , and bartinella eliszabethea . It showed an igm and igg possitive but all my reg lab tests western blots and Elisa were negative :. I am now on treatment again and I’m taking bolouke and courtem . For the babesia right now . I have had sweats , night sweats . Vibrations in my head . Ringing ears . Muscle pain amd joint pain . Chills . Anxiety . Nerve pain . Burning sensations insomnia . And been bedridden for almost 3 years again . The exact same thing happened to me 19 years ago . I am being told by the benzo community that I am still in withdrawals from the valume the phyc drs put me on ? I’m scared and confused because I am off valume now for 3 months and I tapered slow for a year . Not many drs know about eather things . Lyme , co infections or bind “benzo induced Nuerological disfunction . Both things work on the cns . And it’s very confusing . But , I am treating this no matter what Becaise I strongly believe that my pain is from the tick borne illness . I am 46 yea old women . On disability now . And fighting every min . My question always has been . Why is my pcr showing igm positive after 3 years already . That’s why I am going on symptoms. How to know the difference between babesia . Lyme and bartinella . And benzodiazepine injury ?
Hi Jami,
I just wanted to respond because I’m going through the same thing. I’m only 37. I had Babesia Duncani but tested negative for Lyme. I haven’t been on volume or any addictive medicine but have all of the symptoms you have described. My whole life changed. No one understands at all not even my husband. My house is a mess. I struggle to take care of my beautiful children. I used to be so active and strong… Now I can barely get off the couch or out of bed. I’m even having strange bleeding that my doctors are ignoring. I force myself to go to the gym several days a week. I don’t eat gluten and try to be really careful with my diet but I’m still not better. If it wasn’t for God and Yeshua… I’d feel completely hopeless. I’m sorry that everyone is doubting you but please know that you’re not alone. Pick up a Bible if you haven’t already. Read Revelation, then Matthew, and whatever you want after that. People fail each other but God never will. God bless you Jami.
Hi Kimberly,
There is a specific sequence when treating tick borne infections:
1) Borrelia (Lyme) is treated first, using Amoxicillin antibiotic, the treatment protocol is: PO Amoxicillin750mg 3 times a day for 10 days.
2) After the Borrelia treatment you have to treat Babesia and/or Bartonella infections, the treatment protocol is: PO Ciprofloxacin, 250mg 3 times a day for 7 days.
3) To improve the immune system you have to eat two fresh oranges a day, plus one fresh red onion every two days for two weeks.
That is it. Good healing and stay positive.
I have not seen evidence that ciprofloxacin works for Babesia. I typically start with Mepron or Malarone combined with Zithromax.I have avoided ciprofloxacin after having Lyme patients with tendonitis and reports of tendonitis.
What about igenix and vibrant tho? Thought those companies were way better.. and then how does someone know or find out if unwell for years ?
Do you know if Babesia has been found in humans in Hawaii? Also, can Babesia symptoms come and go similar to MS and Lyme? I was diagnosed in 2013 with Guillain-barre but have since had two relapse episodes of extreme weakness and the last one left me with continued weakness, fatigue, and pain. Neurologist said it is not Guillain-barre but doesn’t know what it is and rheumatologist diagnosed me with fibromyalgia. I am beginning to wonder if I had tick paralysis in 2013 and got a rickettsial disease.
I am no familiar with the tick borne issues in Hawaii.
You may want to talk to your neurologist about transverse myelitis or NMO (neuromyelitis optica), although this sounds more like transverse myelitis (TM). I have chronic lyme, recent babesia contraction from a blood transfusion, and transverse myelitis. All of the tick borne infections were from before transverse myelitis so I absolutely know the different symptoms from lyme and TM. What you’ve explained sounds A LOT like transverse myelitis. Did you have MRIs done of your spine and brain at the onset of weekneas/paralysis? Did they find a lesion in your spine? If not, it still doesn’t preclude the possibility of having TM. I’m assuming you had a lumbar puncture (spinal tap). Did they test for oligoclonal bands, protein, and white blood cells? Again, all can be normal and still be TM. Lyme disease is also a known cause of transverse myelitis. Mine was triggered by mycoplasma pneumonia although the lyme and babesia have hindered my recovery. I am incredibly lucky, however, and am one of the 1/3 who will recover to nearly 100%. It’s a disease that’s actually even more rare than Guillian-Barré (only 1,400 cases per year in the U.S.) and there are very few neurologists who are even well educated on the disease. You can always send all of your original medical files from the Guillian-Barré diagnosis to Johns Hopkins Transverse Myelitis Center and they will help give you a diagnosis. If you’re curious if this is possibly what is going on, I recommend the Facebook group Transverse Myelitis Folks (Blue Crew). Just my two cents from someone who has experienced all three illnesses.
Could you please tell me more about your Babesia symptoms? I am recovering from Bartonella but I am not sure if heat sensitivity is due to Babesia. Thanks
21days it’s not enough, they did the same to me and I have been having a lot of pain for 10 years and now I had life treating symptoms, very bad neurological problems. This is really serious, don’t waste your time, you need a serious treatment and evaluation I had Bartonella and nobody realize. Please look for help. Dr. Mozayeni in Maryland knows how to treat this. DON’T TRUST IN DOCTORS WHO THINK YOU CAN BEAT LYNE WITH 21 days of antibiotics.
I was infected as a child in the mid to late sixties. I actually had the rash but LD was not known and we thought it was a spider bite. I had recurring illness (with periods of wellness) in between every 6-8 years. As a chemist, I saw an occupational health provider for possible exposure to paclitaxel in my late 30s. I had very severe illness, the nervous system is the most symptomatic and including petit mal seizures. The doctor recognized I had untreated Lyme disease. From there, i found Dr Sam Donta, who treated me and my children with tetracycline 500 mg 3xday for a very long period. I was on and off the tetracycline for two years, followed by a brief course of Biaxin and plaquenil, which gave me severe Herx, followed by 12 years of relative wellness. Every few years I would take tetracycline for 2 weeks. Then, about 4 years ago, symptoms worsened. I was seeing the drs at Northampton Wellness and still working for several years. Reoccurrence of petit mal seizures then prevented me from driving and I could no longer work. I am now dedicated to working with a more local doctor and hitting it with everything I can. I am 60 and have been living with Babesia, Bartonella and borrelia almost all of my life. I understand why the most common cause of death for people with chronic Lyme disease is suicide. But I fight on.
Right there with you. Pretty sure I was born with it in 67, but, can trace it back to three months before I turned 9 for sure. In and out of flares my whole life. Each one getting stronger and lasting longer, to now, where it just doesn’t go away. Ruined my heart, teeth and more. Been told nothing I can do, yet I still can’t get disability, even for a messed up double bypass. So, I just fight. If that means I filled a water glass for the day, and that is it, I count it as a win. Three years ago, they gave me 2 years to live. So, I am winning!!!!
During a routine blood donation I was notified that babesia PCR was positive. I was bit 1 month prior and my PCP gave me antibiotics as a precaution to contracting Lyme’s. I was told by my doctor after receiving the information from the blood donation clinic that because I was not experiencing symptoms I could not be treated and my body would eliminate the pathogen. I was just tested again 3 months after being bit. I’m now being put on 1 week of medications. Do you think this is enough time to kill this infection? I’ve read places that say min 10 days of treatment. I want to get rid of this parasite sooner than later.
There are often symptoms of Babesia during followup. There are also periods of time without symptoms making it difficult for blood banks to detect Lyme disease. The ten day recommendations for Babesia were proposed based on the original study comparing a combination of Mepron and Zithromax vs Clindamycin with Quinine. They were able to clear Babesia from the red cells. I often find longer patients more effective if symptomatic. Doctors are divided.
After 6 nights of night sweats, chills, headache behind eyes and 103+ fever my 24 year old son received an equivocal result for acute lyme and negative for long term lyme. The babesia test results done by the ER won’t be back for 2 weeks. He has started on 100mg doxy 2x per day for 21 days. Should we be treating for babesia NOW based on symptoms? We live in Massachusetts.
There are sweats from other tick borne illnesses.
Doxycycline for 21 days? Might as well put a gun to the poor guys head and save him a lifetime of suffering. Bring him to a real lyme doc. Tests are garbage.
I had my first lyme test in november and all IGGs and IGMS were positive. Now, I have only one IGM absent, and still have a 5.09 lyme test value. Been on doxy for 5 weeks, malarone for 7 months and zithro for 5 months – do your titers stay elevated even if the lyme is gone? I also have babesia – when do you know when you are well enough to get off the meds. I am good for the most part, but every day around 6-7 PM I get really fatigued. Since it is like clockwork, makes me wonder if it is the bugs anymore, or the meds.
The titers typically remain elevated even if the infection has resolve. Your doctor will have to use clinical judgement including ruling out other infections
Bonnie,
I’ve been treated for Lyme many times and Babesia once. I am “normal” then I, too, have fatigue hit me every day.. right around 4…. It is so debilitating, like extreme jet lag… my coordination leaves and my brain fog settles in. I avoid driving and basically have to get horizontal to read or sleep deeply for a couple of hours… then up for about 2 hours. Then back to restless sleep for the night. I am on no medication. Is this your experience. Nothing I do helps.
I have had patients with Babesia that don’t resolve their illness with a short course of Babesia
My 11-year-old son tested positive for Babesia using the DNA Conexions test. The LLMD we were using only prescribed herbs and they did not work. We need to find another medical professional. What treatment should we seek? He has many symptoms and is missing out on a normal childhood.
I am not certain the significance of the urine test you are referring to. It is challenging to validate each test. You might need to add a doctor familiar with antibiotics for tick borne illnesses. You will also need to work with other doctors to rule out other causes.
I have babesia and lyme and have been treating for six years without much success. It would appear that Babesia is the biggest player in my illness yet, nothing seems to knock it. Not even Mepron and Azithromycin. My Dr. is now putting me on the dreaded Quinine/Clindamycin protocol. In your experience is one protocol better that the other in you patients?
I prefer Mepron and Azithromycin to avoid the side effects of Quinine and Clinadamycin. Nevertheless Quinine and Clindamycin helps some people. Flagyl and tindamax has been considered for their antiparasite effects but the research has not caught up.
I was bit in 2001 and had symptoms since that no doctor could explain. In 2010 after a brain and spinal MRI I was told I most likely had MS due to lesions. In 2012, I was positive for chronic lyme and bartonella and in 2016 tested positive for babesia microti and duncani. I have been treating since 2012 with the worst herxing beginning with babesia treatment in 2017 and ongoing.
My MRI’s are much worse and I am no better. My family thinks it is foolish to continue to treat lyme and the co-infections and that I should go on MS drug treatment. I am really discouraged at this point but not sure if MS treatment will make me worse.
The lesions of Lyme and MS are similar. I urge my patients to include neurologist as part of the evaluation as you weight options.
Two months ago, I tested positive for Babesia antibodies, but the follow-up smear and PCR were negative. I now have recurrent episodes of fever/chills/aches/sweats/headache and other symptoms, each short in duration (12-48 hrs) with rapid recovery after. I fear my physician will deny treatment due to the test results and my apparent good health, and I will continue to have a lingering low-level infection. Will this infection, if Babesiosis, truly resolve on its own?
I have been working as a field biologist in MA (Cape/Islands and inland) for 25 years (= major tick exposure). Amazingly, this is my first known tick-borne disease but most of my coworkers have been ill one or more times. I have found many physicians to be (back then and now) a bit slow to the table.
Thanks for sharing your concern. The smear and PCR can resolve before testing leaving only the antibody test. I would not dismiss a positive antibody test.
My Lyme and Babesia went undiagnosed for a year, maybe a bit longer. I’ve finally completed the abx part of my treatment, and was feeling almost 100% I’m starting herbal antimicrobials soon to clean up the last bits, but the problem remains my Babesia infection has clung to my body quite stubbornly. I just had a chest episode (the crushing elephant sitting on your chest feeling) and it’s been atleast a month since my last one. Why is this parasite so damn hard to ridd my body of??! My biggest fear is I’ll never fully get back to normal.
Thanks for sharing your frustration. Keep working on getting healthy.
I had Lyme Disease 2 years ago and was treated with antibiotics. Recently my bloodwork showed a high indication of Babesia infection, which my doctor said indicated a past infection. I have never felt the same since being diagnosed with Lyme Disease (constant fatigue and joint pain). Can Babesia still be present and flare up? Is it worth following up with a Specialist or Rhuematologist? Thank you for your help.
Joint pain is caused by acute or systemic infection with Bartonella, Borrelia or both. The nasty pathogens can trigger immune responses causing constant joint pain. Constant fatigue is caused by acute Babesia infection, because the parasites can invade the red blood cells causing hemolytic anemia. Short 5 days treatment with Ciprofloxacin can clear Babesia.
Hemolytic anemia typically resolves after the first week or two of the infection. I start treatment for Babesia with atovaquone rather than ciprofloxacin based on the evidence and my experience. I have not seen support for ciprofloxacin.
My doctor wants me to take Zithromax/Mepron combo for 4 months because the life cycle of the red blood cell is 110 days.
Is this necessary? I have having increased brain fog, dizzyness and “spacy” feeling since starting a month and a half ago and it is kind of worrying me.
I had babesia and was hospitalized and treated and retested after treatment.Supposedly I am cured. Why do I still feel totally fatigued and have very poor balance. I have even had to get PT for balance.
The original treatment trial was 10 days for Babesia but those cases were identified early. There are a growing number of case reports where longer therapy and retreatment of Babesis has been described.
When you say identified early what amount of time is this, please? Thanks.
I prefer 4 to 6 weeks. I have found that treating Babesia at the same time as Lyme disease helpful
I had Babesia caught early, major symptoms cleared within a couple weeks, a few mild symptoms have lingered like balance issues and fatigue and are slowly trailing off after several months. PCR, smears, etc. repeated several times all blood work is negative. Feel like everything is on the wane, but how long (typically) does it take to get completely back to normal? Are there any supplements, herbs, etc. that might help? Thanks.
I am happy to hear the major symptoms cleared. Ther are some individuals where they remain ill over time. Some benefit from retreatment for Babesia with retreatment. The trials have not addressed who will benefit from retreatment. Supplements have also been proposed but are also not studied.
I have been fighting Lyme, Rocky Mountain Spotted and Babesia Duncani for approx. 4 years. I have had IV pic line for 1 year. Babesia symptoms as wells as Lyme re occurred 7 months after IV removal. I cannot seem to clear the Babesia. I feel that I have tried nearly everything in every combination with only minor relief of symptoms. Is there anything novel you would recommend for the Babs I cant seem to clear? Thanks!
Your case highlights the difficulties we all face when tick borne issues are a concern. Each case needs to be evaluated individually.
My brother has Lyme, babesia,and bartonella. He suffers every day . Headaches, inflamed gut, passes out,going on for 12 years . Seeing a dr in NY we live in IL . He said he’d be dead if didn’t have treatment .
But nothing stays away. Of course antibiotics. My sister has journal of everything .
He is 59. Strongest person because I’d be laid out . Too long but dr in ny said never seen anyone like my brother. Meaning so sick. I’m so sad he still cooks for people he’s a good one.
It can be difficult to know whether a tick borne infection has cleared. I am sorry to hear he has not recover. He should be evaluated by various specialist to rule out other causes.
Thanks for your comments. They reflect how little we know.
Hello,
I am from the Netherlands. In 2005 I got bitten by a tick and had a bullseye rash. and in 2013, after being sick for over 7 years, they found out I had Lyme disease, Babesia, Q fever, bartonella, ehrlichia and another co infection I can’t remember now.
I had 4 months of antibiotics, Claritromicyn because I am allergic to doxycycline.
But I never got better. Have a lot of symptoms but the most worrisome are the fevers.
Still having high fevers a few hours a day and every night. They go up to 40 degrees. And after that I have it so cold. And than it starts again. This is going on for 9 years already. Is it the Babesia? They never gave me a treatment for it. Because it would clear by itself. And my house doctor doesn’t believe in Babesia. She says it’s a animal disease and I am not a cow so I can’t have babesiosis. The test in the hospital must be wrong she states. (4 years ago they tested me for Babesia two times in a hospital. )
What can I take to stop those fevers? And can Babesia persist? I have it since 2005, and they never treated it.. is it possible that I still have it?or do I need to look for another reason I have those fevers for 9 years. (Can’t be malaria though, never been in a country where they have malaria, and I am only 29 so not menopausal).
You say you are allergic to Doxycycline.
Be careful with that assumption. I have never felt as ill taking doxy to treat lyme and coinfections. I was told categorically that I must be allergic and to stop taking it.
It was actually severe herx and a sign it was the right treatment. It is an antibiotic you can probably titrate, as I had to do. Doing this I was able to build up to much higher doses, much to the surprise of my regular doctors.
Doxy cleared most of my symptoms, but only after they got a lot worse for many weeks. Also be very aware that panic attacks and a desire to end it all can accompany doxy. BE CAREFUL! If you can’t stand it, back right off the dose and start warily.
As an aside, I was dragged on a skiing holiday, staying at very high altitude about 7 weeks in. I stopped taking doxy on the advice of my LLMD. Doxy causes skin sensitivity to light.
I couldn’t believe how much better both myself and my wife were up the mountain. When we descended at the end of the week we both had a short episode of extreme nerve buzzing, like taking the top off a shaken bottle of coke.
Going high up a mountain and staying there for a week seemed to have a profound impact on both our recoveries.
Generally, if a treatment makes you feel dreadful my personal view is that you seriously need to consider that it is a sign it is working! It’s like standing up to any tyrant – it’s going to be painful in the short term and a sign you aren’t going to tolerate it any more.
Just my experience, so please don’t take it as advice – but it may be informative. The very best of luck. There is life after lyme and the plethora of friends it knocks around with!
I have had Lyme starting in 1983 and appreared symptomless after IV antibiotics for 2 weeks hospitalized. I was reinfected in 1992 (new husband) and treated again for Lyme Borrelious and co-infections in 2002. I am having a reoccurrance of Babesia and Bartonella. I took Rifampin 300 mg and Doxy 100mg and got lessened some symptoms – hot/cold, extreme cold extremedies, much mental confusion but since that was completed, I continue with “freight train tinnitis” with loss of hearing, extreme exhaustion and brain inflammation feeling like my brain is larger than my skull.
I feel I need to continue on the Bart meds above but need also the cognitive and brain inflammation addressed. Can you suggest the best antibiotics, strength and duration?
My husband with Parkinson’s diagnosis is showing the same symptoms, he needs this treatment as well, we are not functioning well at all. Thank you for your thoughts, we have spent our savings and are still suffering. Our internist is perscribing our treatment with advise.
I share what I have learned in the published literature and in my practice. Neither Rifampin or doxycycline work for Babesia. It can be difficult to determine the best treatment without a consultation.
It can be complicated when tick borne illnesses are part of the problem. For example, neither rifampin nor doxycycline work for Babesia. It is also important to rule out other conditions.
How do you feel about using malarone instead of mepron? What amount of malarone do you recommend daily?
I have been using Malarone more often than Mepron lately. For readers who are not familiar with the difference, both are based on atovaquone. Mepron is 750 mg per tsp and Malarone contains 250 atovaquone combined with proguanil.
Is a positive antibody test reason to treat symptoms?
The blood smear and PCR are more typical of early presentations. Often the only remaining evidence is an antibody test. The symptoms may not include sweats. You still have to use clinical judgement to decide treatment.
I grew up in northern Westchester county, NY in a deer infested area and it took doctors almost 7 years to diagnose me with lyme disease. My problems go back to the early 90’s. I’ve heard of babesia and co-infections but never knew they could cause all these issues based on what folks in this thread are mentioning so that might be something for me to check out. The infectious disease doctor I saw in New York City sent me to have a SPECT scan of my brain since my big issues were panic attacks, phobias, stomach issues and intense brain fog. Most other docs said it was just hypoglycemia or mono. The SPECT scan showed extreme white matter hypoperfusion and abnormal ‘swiss cheese’ blood flow in my brain. I was put on a home IV for 16 weeks and they tried two different kinds of antibiotics. It didn’t do much to clear my symptoms and the infectious disease doctor said he did all he could and said I should probably just go on SSRI meds for the rest of my life to deal with it. Strange as Xanax does seem to help with the brain fog and panic most of the time. I’ve lived with this for almost 25 years now, but somehow managed to start of successful company, get married and start a family. Hopefully they will make SPECT or PET scan more readily available for diagnosis of these tick diseases so people don’t have to go through what I went and still go through.
Thanks for sharing. It is unclear from your comments if Babesia and other co-ifections were considered as a contributing cause of continued symptoms.
Nah they never tested or treated me for Babesia back in the day. My family doctor here in NYC thinks all the co-infections are BS and that I just suffer from plain old generalized anxiety disorder since I already went to the best infections disease doctor in the country and was treated in her mind. Glad she can get on a subway, fly alone, drive a car alone without benzos, isn’t afraid to get on elevators and doesn’t yell at her wife and kids for no reason. Wish I could say the same. This disease has really ruined a lot of people’s lives so my hope is some consensus on treatment and diagnosis occurs in my lifetime.
Look for David Hunter Group support for Lyme D he could help you. He is a great guy. His daughter had Bartonella when she was a teenager she is heal now and is on her 30’s. For Bartonella Dr. Mozayeni in Maryland. Good luck
I have had these symptoms for 25+ years. Lived in Oregon and Maine spending much time in the woods. Main symptoms, body pain, horrible sweats, vivid wild dreams, depression, restlessness, brain fog, tremor, unsteady balance, itching, increases heart rate and palpitations, chest pain, bladder instability anxiety, fatigue and more. Had to quit my nursing career because I could not deal with the stress. Was framed with diagnosis of Fibromyalgia. Last fall had 6 weeks of severe vertigo and doctor sent blood work to Stanford. Came back with Babesia lab value of 160. Have been put on all the top antibiotics mentioned here, even the Doxycycline. Have felt no improvement at all. If I have had it for so long is it useless to do antibiotics anymore?
Saw a cardiologist for chest pain. Was put on 400mg magnesium a day due to profuse sweating and my chest discomfort has dropped 85%. So that was helpful but feel that five months of antibiotics have not changed my symptoms with the exception of having a bad herxing reactions. Almost died after trip flying from Maine to California on New Year’s Day 2018.
They said my kidneys were dry and said I was in critical condition . My body felt that it was shutting down. I don’t know if I should pursue treatment or accept things as they are after having it so long.
But was hoping I would have improved after that and didn’t. In bed most of my days. My SaO2 in RA is 94. Should I give in to the fact that this is just who I am now.?
I am happy to hear the doctors considered Babesia. It can be difficult to find a solution. You also need to consult other doctors to rule out other illnesses.
I tested positive for Lyme back in 2007. Did 21 days of doxy and was fine. This past Oct I wasn’t feeling well…tested positive for Lyme but the doxy didn’t help this time. I went to a LLMD she has made taking zythromax and malorone along wth allergy meds. I have been feeling better with some bad days mixed in. I have read the symptoms on MS however and can not believe how similar they are to my symptoms. I feel like I haven’t had “classic” babesia symptoms. My worst symptom is I feel a shakey sensation in my head. Some other symptoms been fatigue, feeling sore in my hips when I lay down, air hunger, and anxiety. Should I be doing other testing or is it safe to say this is most likely babesia and/or bartonella. She is treating the babesia currently but thinks we will most likely be tackling bartonella next…
Good Morning Dr. Cameron…
I came across this web page as a result of my search looking into repercussions for having Babesiosis…
I was diagnosed with Babesiosis in July of 2016 (as well as Lyme, have had quite a few times) and had quite a bout with the Babesiosis. It’s a long story as to how I came to be tested though just the same, I definitely had it (or might I say still “have it”). I was blessed that my Emergency Room Doctor knew of the denial game that is going on and had my blood samples sent to California …
At that time, the only suggested antibiotics to take was Zithromax with Mepron, though the insurance would not approve the Mepron because it was not an approved medication at that time by the FDA for addressing Babesiosis (don’t know if it is still not an approved medication for Babesiosis)…
Because the insurance would not approve the Mepron and that the price I was told was ridiculously high, much more than I could afford, I searched the internet for anything else that could be used. I felt that if the insurance wouldn’t approve the medication that there might be other medications that might be available to use against this parasite. That possibly the insurance had something else in mind that they were not mentioning…
I came across a site which mentioned that one doctor had good results with using Doxycycline, Zithromax, and Clindamycin taken together. I was already on Doxycycline for the Lyme (yes, of course I had that as well…lol) and before the Dr. learned the Mepron was not approved had me on the Zithromax as well, it was on filling the scripts for the Zithromax and Mepron that I learned about the insurance concerns for the Mepron. Was approved for the Zithromax so I started taking that with the Doxycycline…
So I mentioned me findings to my Family Dr. who then gave me a script for the Clindamycin as well….
It was a terrible 10 days taking the Clindamycin with the other medications with acid reflux that could kill a bull (oh, did I burn…lol) though it seemed to take away the symptoms I was having from the Babesiosis…
I have a local Infectious Disease Doctor who originally came out of Stony Brook University’s Infectious Disease group. I am not happy at all with the information I received from this Doctor, I seem to get a run around from anyone coming from the group at Stony Brook (I had originally seen one of the doctors there many years ago after my first bout with Lyme, same run around)…
I keep all my record history pertaining to my Lyme tests, both IgG (6) and IgM (2-3) are lit up across the board on the last few tests. I am told now that I will not be tested anymore because the results with be the same no matter what…that I will always show positive now with the western blot using the IgG and IgM bands…
I recently called my present Infectious Disease Doctor about some new tests at this time and was very dissapointed that he had no idea of any (Nanotraps is one, I hope I spelled it right) after I brought this to his attention he then found that the tests are real and most likely not covered by the insurance yet…
I am on Long Island NY and I am wondering if there is more information on dealing with both Babesiosis and Lyme and their aftermath…I am concerned…wait…more than concerned…I feel one or both of these are still attacking my system…
I am a person who is quite tough (or should I say I was)…I am now 62 and can’t tell if my issues are just because of my age or are they related to having these diseases still active in my system…
Please, if you can, help…lol…is there any light you can shed on this…
I thank you in advance for your time and consideration…
Sincerely
Guy Langellotti
Most antibiotics are not approved by the FDA. I don’t believe that doxycycline, amoxicillin, Zithromax or IV Rocephin are FDA approved. Clindamycin combined with quinine has been recommended for Babesia but has more side effects that Mepron and Zithromax. It is not clear that clindamycin works without quinine for Babesia. You may find a lower dose Mepron or oral Malarone might help your doctor. The cost is lower if you can use the GoodRx app.
So what you are saying in that I did not have the Clindamycin with quinine I might still have the Babesiosis? I was only given the combination Doxycycline, Zithromax, and Clindamycin taken together as I stated. Also, is it worth me coming to see you in that your address shows you are 1 hr 40 min away from me. I am with Health First with the Gold Leaf Premier policy? I really am not getting much attention from the local infectious doctors, as I stated, they seem to have a printed statement concerning these diseases.
Guy
I am not convinced that clindamycin works without quinine. You are welcome to call the office agt 914 666 4665.
Hi Dr. Cameron. I found an adult deer tick on me (feeding near armpit) and removed it, and sent it to be tested at UMass “tickreport”. The tick tested positive for Babesia microti. It has been 10 days since I removed it, I am still asymptomatic (I have been feeling somewhat lethargic/depressed, and my arm on that side is slightly sore, but it may not be related). Should I get antibiotics just in case, since early treatment is more able to eradicate it?
Thank you very much!
Gabe
I am always concerned when my patients have any symptoms within 6 weeks of a tick bite. Babesia may take awhile to develop symptoms. see my blog at https://danielcameronmd.com/blood-donor-infects-premature-infants-babesia/ I can’t give individual advised without an office visit. You should consult your doctor given the symptoms even if they are not so clear cut.
I used to go to you, Dr. Cameron, for treatment, but since I am very far and do not drive long distances and feel so very sick every day, I don’t know what to do. I tested positive for Lyme and Babesia microti, but recent tests from regular pc came back negative for both; I believe they used any old lab. I suffer with joint pain, night sweats, stiffness, constipation, heartburn, but MOST OF ALL SOMETHING I NEVER HEARD ANYONE MENTION, I HAVE CONSTANT BURNING LIKE A FIRE INSIDE MY ANAL AREA, 24/7, ALL DAY. gASTRO SAID IT MAY BE PUDENDAL NERVE DAMAGE. i HAVE HAD SHOTS FOR pn with no success. Have you heard of Babesia microti causing this burning, from any of your patients. Some doctors have told me I am a psychopath with all these strange symptoms, especially the burning sympton. It’s like having a fireplace lit inside my rectal/anal area.
Sorry to hear you remain ill. I have not seen the pain you describe. Perhaps others have. It sounds as if pudendal nerve blocks have also failed. Keep working on finding a solution.
Last August I was sent a letter from the RI CDC that I was infected with B. Microti, recognized after a blood donation. I believe I was infected early summer. After convincing PCP to test , got tested in OCTober, smear neg. PCR was positive, serology not performed, and not given treatment. Pursued PCP due to symptoms, though not debilitating but present and affecting quality of life. Retested in Feb., smear was neg, PCR was neg, antibodies in sereology were 256. Granted treatment of Zpack and meprone. Felt good for a couple of weeks. Fatigue and joint pain resurfaced, more than before. pursued more blood work. Smear and PCR clear. Antibodies at 64. PCP declares success. I think otherwise, do symptoms still appear after a successful treatment? Is a second opinion recommended? Will this clear up on its own? Is bloodwork the holy grail of diagnoses? Aargh, its frustrating when you live in ground zero for these infections and you would think there would be more knowledge about them. You make an inquiry but all you hear is crickets. I asked the CDC director in the beginning via email if there were any research I could get involved in but she said she did not. It all seems strange to me. Sorry for rambling and there are those who are much worse off than I, just needed to vent and this seemed like a good place.
I am happy to hear your doctor has worked hard with some success. It can be difficult to resolve the illness. Sometimes a change in treatment to include Babesia is helpful. There is no test to verify an infection has resolved. It is also important to rule out other causes. I typically have to do a complete evaluation to look for opportunities that might have been overlooked.
Hello Dr. Cameron and fellow lyme peeps : )
No lyme disease for me as I can find from past ELISA and Western blot test but a recent blood work on me included a Babesia Microti Anti Panel test, and came back positive on the IgG @ 1:80. I suspect infection happened back in November 2013, but can not be sure.
My Dr wrote me a prescription for 42 -100mg doxycycline capsules to be taken 2 times a day. But from the info here and elsewhere that is not the antibiotic that is normally used for babesia. When i questioned him on his choice of antibiotic he stated it was the normally prescribed antibiotic for babesia. I will be seeing a LLMD that is listed with the ILADS organization in about a week for a second opinion on that. 1 1/2 hour commute but it is very important to me to get this right.
Severe headaches on the left side along with many of the other reported symptoms for me. I am a bit worried about my 55 year old kidneys feeling the strain of the last four years. I was miss diagnosed with cluster headaches and migraines by various neurologist and previous family doctor.
I was very pleased that a new family doctor agreed to include various lyme co-infections tests with latest blood work. But was confused by his doxycycline script. I am thinking of picking up the doxycycline anyway or should I wait until I see a LLMD?
Thanks
The best treatment for Babesia is a combination of Mepron with Zithromax since the article by Krause PJ1, Lepore T, Sikand VK, Gadbaw J Jr, Burke G, Telford SR 3rd, Brassard P, Pearl D, Azlanzadeh J, Christianson D, McGrath D, Spielman A. in the N Engl J Med. November 2000 Nov. called Atovaquone and azithromycin for the treatment of babesiosis in https://www.ncbi.nlm.nih.gov/pubmed/11078770
Until then quinine and clindamycin had been preferred. Some have used a lower does Malarene for Mepron for the atovaquone.
That’s interesting about kidney disease being associated with babesia. I didn’t know that. I have babesia, Lyme and bartonella. My kidney function test showed low filtration since at least 2015. GP’s and Internists don’t even mention it until their patients are critical and need dialysis, but my LLMD, who is a functional medicine doctor, was alarmed enough to suggest that I might need to see a kidney specialist. She also suggested I take Trizomal Gluthatione liquid, which can help heal kidneys. After a couple of months of that, my last kidney function test was normal, for the first time in two or three years.
I have not seen renal disease in Babesia. I understand renal disease is common in dogs.
You are right, because dogs are Bartonella carriers, Bartonella can cause kidney, eye and heart damage big time. You can be infected via tick bite or dog bite/scratch.
I have had Lyme several times over the past 20 years and had a doctor that specialized in the treatment of it. He has since retired from practice and my present Dr does not support long term treatment. I have tested positive/inconclusive for B. microti and cannot donate blood. My question is has there been any research on using colloidal silver? I used it with the antibiotics with the first Dr and told him and he said there was no reason to think it would not work as it was used to treat syphilis.
I am not familiar with the research on colloidal silver. I assume your treatment included medications for Babesia.
I was diagnosed with Branch Retinal Artery Occlusions in April 2018 and Babesiosis about 6-weeks later. I have Hollenhorst Plaques in the Occlusions. I am 40 and do not have high blood pressure, high cholesterol, my echocardiogram and carotid doplar were good. I saw a hematologist and there has been no indication of a blood clotting disorder. I underwent a stroke assessment with an MRI/MRA and that was clear. I have severe fatigue, night sweats, chills, elevated temperature, excessive yawning after being up about 6hrs, and sometimes day sweats. My PCP prescribed the anitibiotic/antiparasitic that the CDC recommends. I am thinking I should see an Infectious Disease Specialist for the Babesiosis. Could the Babesiosis cause the BRAO or contribute to aortic issues that may have released the plaque? I also have a history of illness and less effective immune system. My PCP was thinking my case was mild, but I’m wondering if there is more cause for concern? Thanks for your input
I have not seen any information to address whether the retinal or aortic issues are related. There are doctors who are reluctant to treat Babesia unless the parasites are seen in the red cells and then only for 10 days. Doctors are divided on their approach to Babesia.
Back in January of this year, after multiple trips to urgent care and my pcp over the course of 4 weeks, I was finally diagnosed with Lyme and Babesiosis. I was treated with Doxy as well as Atovquone and Azithromycin for 10 days. Within 48 hours the majority of my symptoms had cleared up. Now, 6 months later, I am having the same symptoms, but they seem to be worse. It’s only been a week, but the headaches are crippling sometimes, and the fatigue is so bad I have a hard time making it through a day just sitting at my desk.
I feel like it must be the Babesia again, as the symptoms are nearly identical. My doctor is hesitant to treat me without my visiting an ID specialist. The only problem is it would likely be 3-4 weeks before I could visit a specialist. I feel like I am barely functioning, and don’t think I can handle a month of this again.
The original paper proposed ten days of treatment. Their cases were treated early. There are cases in the literature where longer treatment was required. I treat longer when clinically necessary.
Hello Dr Cameron,
I’ve been searching for years (close to a decade now)for a doctor that can help me in the Houston area. I’ve been told that I have fibromyalgia, but my symptoms are so much more and keep getting worse. After 20 years in dentistry, I had to stop because of severe pain and migraines. I started to suspect Lyme after my mom was diagnosed and those close to me said my symptoms matched. The deeper I researched, the more I realized I have/have had every symptom on rhe chronic Lyme list as well as other coinfections. The last neurologist I saw would not order a blood test for Lyme or any coinfections because he said it is not here in Texas. So I ordered a CD -57 test online. It showed numbers for chronic Lyme. When you take this into account as well as symptoms that could fill up a page if I listed them, I need to find a doctor in this area that is a LLMD. Do you know of any here in Houston/Cypress/Tomball/Katy/Sugarland? (I can go several different areas.)
Greatly appreciated,
Hilary
You could contact ILADS, the global Lyme Alliance, Lyme Disease Association or LymeDisease.org. You could contact a local support group. You could also fly to New York if all else fails.
Dr. Cameron
Can Babesia be cured without treatment over time and a strong immune system? I recently tested positive to ALL bands on western blot. I believe I was infected in 2009 when I was violently ill with a “flu” that lasted several weeks and since then, I continue to get the same familiar achiness throughout my body and last summer was sick from June-Sept with “5ths disease”. In April of this year my knee became double in size which finally resulted in a lyme test ….. I am now on my ninth week of doxy with two doctors that admit this is not their area of expertise…. I do not want to be treated with a PICC – waiting on more test results of the fluid from my knee since I understand the fluid is a better test vs. blood / western blot will always show positive even if very old…. by the way I am located in upstate NY.
I often have patients who find Babesia to be part of their illness. They often find they don’t get better until they get treated for Babesia. Doxycycline does not work for Babesia. The knee fluid typically negative doxycycline even if the symptoms and knee swelling persist.
Thank you for your quick response. Are you saying because I’ve been taking doxy, the knee fluid will be neg. even if active lyme? My doctor said I have old antibodies to babesia but not currently active – she did a lab order for Babesia Microti DNA, QUAL, PCR, Unspecified Specimen and Babesia Smear, Blood . I know results can be false/neg and feel confident I have it and need to be treated for it – do you take lyme patients? Where you you located in NY?
The smear clears quickly. It is not clear how often the PCR picks up Babesia.
A positive IgG antibody test for a virus typically means the virus has cleared. The best know exception is HIV where a positive antibody test does not mean the virus has cleared. The same goes for a tick borne illness. A positive antibody to Babesia does not mean the infection has resolved. Nor does a positive IgG western blot for Lyme disease mean the infection has cleared. I am seeing patients in Mt. Kisco, New York, 35 miles north of New York City. Call 914 666 4665 if you have any questions.
Thank you for sharing your knowledge. I appreciate the information very much!
If you do not mind, may I ask one more question – is there ANY way to determine if the virus or confection has cleared?
Also, (sorry, more than one question). I’m being treated for the lyme with Doxy (12 weeks now and still having knee issues) – should I be treated for Babesia at the same time or stop the doxy and then start on Mepron & Zithromax, for example (as I know you are unable to suggest without seeing me in person). Thank you in advance for your opinion…. I need to be smarter than my doctors because they do not know…. admittedly. 🙂
We do not have tests to determine if tick borne illnesses resolve, yet. Your treatment plan will depend on the doctors assessment e.g. have other infections resolved.
Dr. Cameron:
I’ve asked this question to my pharmacists and others and can not seem to get a clear cut answer – Is it okay to use an infrared sauna while taking doxy?
I do not know if the light from an infrared sauna can lead to a photosensitive reaction.
My son and I were each bitten, him by an Ixodis larva or nymph, and me by an adult dog tick, 2 days ago, while vacationing in Long Island, NY. Far in country, we had no tweezers, and had to remove both ticks by hand, with some squeezing of tick bodies unavoidable. I think we got each out looking intact, in less than 24 hours, but worry that each tick body got squeezed during removal.
Dr. Cameron, my question is: how soon can we test for tick-borne pathogens, and which tests would be best? Thank you so much!
The tests will depend the clinical presentation. The tests should assess for other illnesses. The tests for Lyme disease often take 3 to 6 weeks and then may not become positive. The time for other tick borne illnesses is less clear. Your doctor may have to use clinical judgement.
Dr Cameron, I am being treated for Babesia (Mepron / Zithromax). I started feeling better within ~9 hours of starting antibiotics. I also tested positive for Lyme. Initially I convinced my Dr to start the Babesia treatment before tests came back. All of the symptoms were a perfect fit including ultrasound of liver and spleen (enlarged). He agreed enough to prescribe the two drugs, but only 5 days initially. Now it is time to prescribe remaining treatment and he was prepared to only add 2 days. I explained most updated literature talks about individual clinical assessment to determine length of treatment. I also mentioned, per what you’ve written here, that the papers on the drug combo were written using a 10 day protocol. He is open minded and asked me to provide him links to the papers that show this. Can you provide me with supporting documentation that will satisfy a medical Dr so he doesn’t cut me short of a full recovery? I am doing better, last night and this morning first time in 5 days I haven’t had a fever. Still have headaches (less severe). I just want a full recovery.
https://www.nejm.org/doi/10.1056/NEJM200011163432004?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dwww.ncbi.nlm.nih.gov
Thanks for this site Dr. Cameron. My 88 year-old Dad was just diagnosed yesterday with Babesia after going through a month of feeling awful – nausea, headaches, fatigue, loss of appetite, anemia, etc – I was concerned we might lose him. He’s been better the past week, so the Dr. who made the diagnosis – his former oncologist (Colon cancer in 1993) – didn’t prescribe anything. I wondering if that is the best approach or whether it might be wise to have a treatment of Mepron with Zithromax. Your thoughts?
I cannot evaluate a patient without a clinical evaluation. I typically look a second time for subtle symptoms before dismissing Babesia. There is also a potential for a clinical presentation if your 88 year old Dad gets old or immunocompromised.
Dr.Cameron
Test order: Lyme Ab/Westeren Blot Reflex
IgG P39Ab,P41Ab, P45Ab Present
IgM P23Ab, IgMP41Ab Present
Lyme IgG WB interp. NEgative
Lyme IgM WB interp. Positive
Lyme disease Ab, Quant, IgM. Equivocal 0.97
Lyme IgG/IgM Ab. Equivocal 0.91
QUESTION? DO I HAVE LYME?
Your tests are supportive. Your doctor will have to look at the entire story including symptoms. They will also have to evaluate for other conditions.
I was just treated for Lyme for 4 months with Biaxin and Amoxicillin. I’m still not feeling well. My doctor thinks it’s Babesia and want me in Mepron. Will that antibiotic alone do the trick? I really don’t want to go in Biaxin again.
Mepron is my preferred medication for Babesia in my practice. The Krause paper used Zithromax rather than Biaxin with Mepron. I have used other approaches in my practice when needed.
My physician is suspecting Babesia. However, I do not have the lab results yet. I never saw a tick on me. I was on a 2 month course of Minocycline and Azithromycin. We did not continue that due to chest pressure. I had to go see a Cardiologist. All Cardio tests were negative. I had a brain MRI without contrast that a Neurologist states it shows periventricular gliosis. He is assuming MS but is unsure. I have night sweats, low grade fevers, insomnia, and I am very dizzy everyday. All autoimmune lab tests were negative. I do weight training and I’m a runner. Lately I can’t run because I become very lightheaded and feel as if I may pass out. My doctors, internal med, Cardiologist and Neurologist say I can continue to workout and run to whatever my tolerance allows. Is it bad to push through the dizziness and could I be causing more damage to my brain this way? I can push through weightlifting without the feeling of passing out. I can run 1/2 mile and get so lightheaded that I feel like I may pass out. I walk it off until I’m good again and I’m able to keep running. Could this be causing more problems for me? I usually feel pretty good after the run. I’m 38 and have always been healthy up to this point.
Hello,I have been suffering from kidney and liver damage after an unsafe sex.I couldn’t find the reason.Could it be babesia or other pathogens?
There are far too many causes of kidney and liver damage. You should work with your doctor with and without specialists to find the cause.
Dear Dr. Cameron, First thanks so much for your valuable time helping patients with questions. I have had Babesia Ducani for many years now. I have been treating with “Coartem ” the last 6 months, but NOW trying to trick the parasite and go back to Malorne. I Continue to show a “high load” of Babesia Ducani at Igenex Labs. I am now 71 years old……..and seriously considering “Red Blood Cell” Exchange Tranfusion due to my age. I know of ONE LLMD in Puerto Valarta, Mexico that does this and has excellent results with difficult treatment resistant cases of Babesia….especially “Cerebral Babesia”…….what is your professional opinion on this matter????
I do not have any experience with exchange transfusions. On paper describe the successful use of exchange transfusion in an asplenic person. The case was early.” His peripheral blood smear showed features of B. microti, with a parasitemia of 28.5%” writes the authors. The journal is at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5144532/ I do not have the information to evaluate exchange transfusions without parasitemia.
My daughter..age 9… last year was covered in the tiny ticks and i took her straight to our pediatrician two days after when she developed large pink filled in circles.. we were sent home with nothing!! 6 weeks later she got very ill..neck,joint pain,lethargic,large r ash on back of leg,leg tremors.. sooo awful.. we went o C. Barnwell, from Georgia and did 9 months of cefdinir and azythromycin along with lots of natural herbs..etc.. we moved to the beaches of Florida to escape the HUGE amount of people that are getting tickborn illnesses in coweta and fayette counties..Georgia.. its been 4 months since we moved and stopped treatment and she is getting faily headaches with eye pain.. left side top usually..clear eye exam and mri.. infectious disease dr was rude and said theres “no lyme in GA.. could these headaches be erlichia,bab or lyme?? she is 10 now and were not sure what to do or id this is tcik born related..whats your guess?? shareen
There are many cases of Lyme disease in the South including Georgia that are not reported. I look a second time for Lyme disease in my patients. Perhaps there is another approach. I also add specialists to make sure I do not overlook another illness.
My son is 9 and started having tics in 2015 following a strep infection. We recently had him tested to see if his tics were caused by the strep and we also had him tested for lyme. His Elisa tests came back negative but his western blot was IgMAlt positive for Igm 41,34 and IgG 93/83,41. We also received blood work for babesia microti by IFA negative IgG positive IgM and anaplasama by IFA was negative IgG and IgM positive. Does those tests mean he has lyme,babesia and anaplasma? Also the dr wants to treat 2weeks doxy and 1 week alinia along with herbs. Thoughts? Does he need to be treated with those results and if he does is that proper treatment?
I cannot make a diagnosis without seeing him. I have patients with all three of these conditions. I generally treat longer and base my treatment on response. I also use that time to rule out other illnesses. I prefer Malarone if I am considering treatment for Babesia.
It’s taken 16 years to find out what’s wrong with my 18 year old son. Full blown 10 years ago after 2 weeks of the flu. Doctors thought I was crazy and he was “functional “. I was beside my self because last year he started having tremors throughout his body and seizures. SPECT shows like an 80 year old dementia patient. Had a positive Babinski sign and Neuro did an MS work up. Now everyone is worried. After having an expert out in California look at his scan he recommended a dr because his brain looked like a virus was running through it. He tested positive for Babesia duncani and indeterminate for Lyme Borrelia, positive for HHV6. He is currently on Atovaquone, valganciclovir, Azithromicyn. We are going to switch him to IV since he has UC as well, probably from the the babesia and worried about absorption. It’s a shame that I have been to the best hospitals to have get to this point. I’m so worried about him not getting better. He handles it so well because he’s been dealing with it for so long. I don’t know if his brain will get better or if the damage is done. I just want him to be able to live life. He’s unable to do anything. Cognitive skills have declined, memory issues are the worst, neuropathy, headaches, muscle pain, Costochondritis, tinnitus. Just want some peace for him.
Hi Dr. Cameron, my 16 year old daughter is being treated for babesia with a protocol of malarone and zithromax. After 1 month, her LLMD wants to add Coartem to the malarone (and ditch the zithromax). All the Coartem protocols I have seen are several days on, then time off; her LLMD wants to use malarone and Coartem every day together. What are your thoughts on this approach? Thanks for your answer and for your valuable website.
I prefer staying with the Malarone and zithromax for my patients.
Good to see someone finally mentioned B. duncani, which is becoming more widespread and can be even nastier than B. microti. Perhaps the former deserves some specific commentary from you, Dr. Cameron.
Doctors have focused on Babesia microti in the East and Babesia duncani in the west. The eastern researchers have typically not looked for Babesia duncani in the east. I do not believe New York allows IGeneX to test for Babesia duncani if ordered by a New York Doctor.
De Cameron thank you for this insightful content – you are helping so many people with this information.
I’ve been struggling with fatigue, headaches and brain fog for the past 4 years and have seen over 12 specialists – only today did I test positive for babesia fish and duncani IgM.
What kind of doctor should I see to treat this?
Will I get better? Or are chances of the medication working slim?
Thank you
I commonly see patients in my practice who have been evaluated by a wide range of well trained doctors who are still ill. I would look a second time at a tick borne illnesses. I often find treatment for Babesia helpful.
Thank you for all your info. Its takes a special person to spend time to answer questions. My question is simple.. i was tested for bartonella it shows a low reading, but not high enough to be postive. Can you still have bartonella. this test was taken 1.5 months later after being diagnosed with lyme. I had 5 out of 10 bands and 3 out of 5 bands. it started with a rash, headaches, pain up and down my back and stomach area then bells palsey, After 3 weeks of treatment all pain went away.. however. I get humming in my head it goes up and down based on my stress level, that was after a month after first doxy. I was treated with doxy… for 3 weeks and then lyme support spray, then i decided a seeing a lyme doctor, he put me on doxy, flagyl and varacycvior for 6 weeks.. I complain about the humming so my lyme dr. put me on mincycline and clarthromycin for another month to see if bartonella was the cause of humming .. after a month of take the min and clar… humming has not stopped. So i wondering if lyme is still around and humming is from my anxiety of being scared with lyme for 6 months… I still wake up fearful, but after exercise the fear goes away.. my fear is taking all the meds i guess
It is common to find evidence of more than one tick borne infection. It can be difficult to determine which infection plays a role. It sounds as if your doctor has considered more than one infection. It is difficult be sure the cause of your humming. You have to also be evaluated for other illnesses. Humming can be more frustrating than people imagine.
I have read that Babesia can persist in the miles of tubules in teeth. I’m asymptomatic. What risk is there of Babesia (or Lyme, Bartonella) re-emerging after dental work, cleanings, oral surgery, periodontal procedures. And is there a benefit to involving the dentist and opening up the can of worms unnecessarily?
I am not heard of the problem.
Sandy,
I had retinal occlusions as well. I have chromosomal disorders of the blood but not necessarily the cause. One evening, my right sideof my face was psrtially paralyzed and was experiencing numbness and tingling in my right arm and right leg. The er dr diagnosed Herpetic Neurolgia. I have not been able to work in an office. I am fatigued w sporadic high fevers/night sweats, headaches (right eye ) and joint pain. The clinical diagnosis is Bartonella in addition to thr lsbs that showed babesiosis (duncan) and Anaplasma. Try Bartonella?? Good luck.
Dr. Cameron, you share that you prefer Malerone to Mepron these days in the treatment of Babesia… Just wondering if you usually include Azith. along with the Malerone. I’ve read both, that it’s only necessary to use with Mepron, and not with Malerone. Your thoughts — with or without? Thank you.
I typically use azithromycin with Malarone as described in the original study. I will start new patients with doxycycline and Malarore in new presentations if I need to cover Ehrlichia and Anaplasmosis.
What dosage of azithromycin? Also is doxy the best for ehrlichia? I previously took a combo of minocycline and tinidazole. Thank you
I typically use azithromycin 250 one a day for my patients. I find doxycycline to be the best for Ehrlichia. I determine the best treatment on an individualized basis. I also need to be sure my patients do not have an another illness.
Dr. Cameron, in your experience does babesia ever cause a tingling or burning sensation in the feet? I’ve been treated for bartonella and Lyme in the past, although my doctor doesn’t believe babesia is one of my problems. I’ve made some improvements in the past year but I’m starting to wonder if babesia could be the cause of my lingering daily headaches (feel like a pressure around the head) and tingling of the feet (usually occurs after activity). I also have been finding small bruises on my legs that come and go without any seeming cause. Could it be worthwhile to investigate babesia again?
It is hard to determine which symptom is related to which tick borne infection. It is also important to make sure you are not overlooking another cause.
Dr. Cameron I am impressed that you have been answering these posts for years. I was diagnosed with babesia and lyme in 2015. I did spend a week in the hospital and was interviewed by the CDC and answered many questions while being hospitalized. I was quite ill for a few weeks, was told I had an enlarged liver, went through a spinal tap procedure and plasma transfusion but seemed to recover fully after 4-5 months. Why do I keep reading of people suffering from tick borne diseases for years yet mine seemed to run a natural course? Are there long term affects I may be ignoring?
I have many patients who doing well. I also work with patients who are not doing well. Thanks for sharing.
Hi Dr. Cameron, thank you for providing your valuable knowledge to those of us who are in need. You are amazing! I’ve been treating Lyme and Babesia (as well as parasites, mold, and metals) naturally for 2+ years after an initial 4 months of antibiotics that made me feel worse. I think I’m very slowly gaining some ground but I’m worried that I’m heading into the dreaded autoimmune response / stage 3. My Naturopath recently prescribed 14 days of Mepron. I’m wondering if this alone (ie without the Azithromycin) is enough to help or am I wasting my money (at $280 with insurance) or potentially creating other problems? My main symptoms include intense fatigue, weakness, body ache/pain/stiffness, insomnia (incl. waking up in panic), breathlessness, tinnitus, and some night sweats. Thank you for your kindness.
I often prescribe Malarone. Malarone still has 250 mg atovaquone rather than 750 mg of atovaquone in Mepron. The cost can be as low as $130 for one tablet twice a day for a month using the GoodRx app on my smart phone. I generally use Zithromax with Malarone as described by Krause. I treat longer based on response to treatment. “Air hunger” has been described in Babesia but has yet to be studied. We need trials. Get better.
Hello! Can you have Babesia or bartonella without actually having Lyme?
The tick can harbor multiple infections. It has been difficult to be sure which infection or combination underlies an illness. For example, Krause treated with Zithromax and Mepron as his Babesia cases also were ill with Lyme disease.
Thank you! I’ve had Negative Elisa, PCR and western blot. All by conventional medicine. I’ve been sick for 6 years. Could there still be Lyme or co infection possibility?
Yes. You also have to rule out other causes.
Hello Dr.
My husband was diagnosed with Lyme disease and Babesia in January after being sick for nearly 9 months. He was on a 4 month regimen of cefuroxime and azithromycin plus atovoquone and now he’s just switched to doxy and cefdinir.
Although he still has bad days we’ve been discussing the idea of getting pregnant with our second child.
Can you give advice as to whether his diagnosis or treatment may negatively affect a developing fetus? Could there be behave genetic implications?Should we wait until treatment has completed? I’m in my late 30s so I hesitate to wait too long but I want the best chance for our child.
Thank you
I have not seen evidence that a man getting Lyme disease affects the fetus unless woman gets infected. I generally bring in the mother and father into the office to make the best decision.
Patient #1 – My ex-husband has been treated for Lyme since last summer. He’s been on antibiotics since then (two). He feels better but began suffering from neurological issues effecting his speech (sounds like he’s had a stroke), swallowing, and now breathing. His doctor, whose whole practice is Lyme patients, (we are in northern Vermont) is now trying to rule out ALS but things aren’t looking good, no matter what the cause is. He drools in his sleep, bites his cheek and tongue when he eats, can’t laugh (or cry) normally, can’t whistle, gets short of breath with minimal activity. His brain works just fine, he seems healthy in all other ways. Has had every scan, x-ray, blood test, trip to the neurologist, speech pathologist, etc. you can imagine without finding any other cause. He’s just started hyperbaric therapy. My question is – does Lyme look like ALS often? And if it is Lyme and not ALS, do these symptoms sound normal? And if so, any thoughts on recovery from the neurological damage? He probably had symptoms for 2 years before he was diagnosed. Never was aware of a tick bite.
Patient #2 – My partner now! Just got a slam dunk diagnosis of both Lyme and babesiosis. Knows he had a tick bite with the bulls eye about 5 years ago. He hasn’t felt well for a couple of years – finally dealt with it. Has all the typical symptoms of babesiosis. Has been on doxy and azithro for 5 weeks. No improvement, perhaps feels worse. Lots of muscle and joint aching – fatigue. (He’s a hard physical worker). What’s the die off like for both or either and how long might it last? Is tinnitus a typical symptom (but he also is on a CPAP machine – and the tinnitus started soon after – but same time as the Lyme symptoms)? And! What’s your thought on Lyme being sexually transmitted?
Thank you!!!
Patient #1 I have seen cases where Lyme disease has been considered in someone that has been diagnosed with ALS. I have seen patient’s “stroke” like speech be related to bulbar palsy of ALS. I have seen gains in some of my patients some times but am unclear if the gains might be in patients with both Lyme disease and ALS.
Patient #2. I don’t find Zithromax and doxycycline alone effective for Babesia in my patients. Ear ringing is common in my patients. I am waiting for more research on the sexually transmitted question.
Thank you Dr. Cameron for your time. I have Bartonella (from a cat scratch in 2010), then a tick bite with classic lyme in 2013. I couldn’t sit for more than 20 min without walking around or lying on the floor from extreme low back/sacro-illiac pain. I improved SIGNIFICANTLY on levaquin in 2015 (not via llmd, but my general practitioner as a trial to see if I had bart as IM rocephin didn’t do anything), then stopped all antibiotics for 2 years only to relapse since I didn’t have an llmd yet. I have been treating with an LLMD for the past year and a half, and none of the current antibiotics seem to be moving it like Levaquin did, though progress has been made. Supposedly the Lyme seems to be more in check and my remaining major symptoms include the classic bartonella symptoms. My neurological ‘lyme’ symptoms have melted away. I’ve been cycling multiple antibiotics – Clindamycin, Biaxin, Rifampin, Plaquenil, Doxy, Tetra, Mepron, Zithromax. Though I have had some “blue sky” moments here and there and progress definitely has been made, I still feel pretty terrible in 3-5 day cycles with only short breaks in between. Levaquin worked VERY quickly and didn’t seem to have the die-off or blebbing and long drawn out pain that I’ve had while treating this last year and a half. I also do not suspect other problems to be too serious because of how many of these big symptoms Levaquin ‘fixed’ last time. Do you find bartonella to be tricky to move? I know Levaquin has its risks and is usually considered a reserve agent…I just don’t understand how it worked so quickly for me a few years ago without terrible herxing compared with long treatment on these other antibiotics. I feel like these other antibiotics aren’t working as well as they aren’t leading to the level of symptom relief I experienced previously. Do you find bartonella to have a tipping point and once you reach that point and clear it from all of its niches the major symptoms disappear?
I am happy your neurologic issue have improved. I am not a fan of cycling. I find it hard to know if Bartonella is the cause even if Levaquin was helpful. Doctors are reluctant to prescribe Levaquin as it can lead to tendonitis.
Treated 9 mo ago properly for lyme and babesiosis. Sx free until 2 wks ago. Now having exertional sob, night sweats, chest pain in midline (like I can’t fully inhale) intermittent abdominal pain, anorexia. 65 y/o in good health. Should I get a CBC or other bloodwork?
You should be reevaluated. I include a second look at Babesia.
Is there any substitute for clindamycin in quinine treatment as I am a high candidate for cdiff
C. difficile can occur with any antibiotic for any condition. I prescribe probiotics with the hope I can prevent C. difficile. I prefer Mepron/Malarone with Zithromox.
Hi Dr. Cameron,
I just received a “past infection” result with Babesia antibody IGG of 1:64 with no positive results for Lyme. Sounds crazy but I am happy. For the last 2 years I have suffered with what my neurologist and GP believe is atypical trigeminal nueralgia and occipital nueralgia of my right side. On anti-seizure meds for the nerve pain but don’t really help much. I have had extreme facial and head pain, bouts of extreme vertigo, pain in my neck, head and shoulder, achy right side of my body and fatigue (I need sleep!) Could this “past infection” result be what has caused this? I am hoping that I could be on a path to finding out what is wrong with me. Seeing an ID in a month. Could Babesia be causing these symptons? Thanks for your thoughts!
A positive IgG typically means a virus has cleared. AIDS is an exception. I am not convinced a positive IgG for Babesia means the infection has cleared. I would look again at Babesia.
I have a IgG of 1:256 for B. Duncani WA1, does that mean I have babesia? I live in N.Y.
I have had terrible joint pain and also body jerking and twitching for a few months.
Babesia microti was first identified on in the eastern USA. Babesia duncani WA1 was first identified in the western USA. I don’ feel they have looked for B. duncani in the eastern USA. I have seen doctors in the eastern USA whoo have dismissed the b. duncani. I have seen positive B. duncani in the eastern USA. I use clinical judgment to decide who to treat.
Hello Dr. Cameron. I got Babesiosis in 2017 on Long Island- experienced fatigue. appetite and taste loss, the start of liver shut down, hallucinations. I was in the hospital three days, but fully recovered. I was back working in two weeks. I know I dodged a bullet- but am starting a short documentary on the subject of tick diseases like Babesiosis. I enjoyed your well researched article.
Thanks.
Are non-epileptic seizures that last hours consistent with the symptoms of B. duncani? We are based on the West Coast.
I have seen non-epileptic seizures on the East coast. I am not sure what tick-borne pathogen or pathogens are involved. I also work with specialists to rule out other causes.
I tested positive for B. microti IFA – IgG with a score of 160 from a IGeneX test but Lyme was negative. My symptoms are shortness of breath, light headedness when exercising, greatly decreased performance exercising, intermittent low oxygen saturation levels while exercising. Had a complete and extensive cardio and pulmonary workup with no issues found. I also have intermittent bouts of extreme fatigue, My doctor recommends 3 months of Zithro/Mepron. Is that one test and these symptoms enough to reach a diagnosis?
I use clinical judgment to diagnose Babesia if other conditions are ruled out e.g. cardiac and pulmonary. I determine the length of time I prescribe Zithromax and Mepron based on response to therapy. I follow incase another illness emerges.
Can babesia be transmitted from a flea? Thanks
I have not seen any information on the subject.
I was diagnosed with Lyme and Babesia in 2005 months after contracting them. After over two years on medicines , I was symptom free and tests came back negative for both. I am wondering why I can’t give blood, 14 years later, when I tested negative for Babesia?
Any answer to my original question?
The professionals responsible for protecting the blood supply are reluctant to allow someone with a Babesia test to donate. This may change if we were to develop a reliable test for Babesia.
Hello Staci, which medication got you cured for Lyme and Babesia? Thank you in advance!
Hello Dr. Cameron~
Thank You very much for all you have done to speak truth to these topics. My husband had typical babesia symptoms for 18 months, then babesia was visualized via FISH test, treated with zith and atovaquone and symptoms abated. Unfortunately, no other co infection tests were completed because in the same time frame, he was diagnosed with primary immune deficiency. Extreme t cell dominant inflammation seen in lymph nodes and liver lead to liver failure and eventual kidney failure followed. A liver transplant was followed two months later with the return of this inflammation with pathology has ruled out as not typical of “auto immune hepatitis.” Both transplanted liver and kidney are now showing same unidentifiable inflammatory processes. Any known relationship between babesosis and this type of inflammatory attack on organs? The infectious disease physicians at this institution denied the validity of the babesia FISH test, treatment was provided by an LLMD. Now that he is post transplant we are compelled to comply with the transplant center physicians but want to ensure that we also explore all options to address potential infectious causes of this inflammation.
Any pointers on where to explore would be appreciated.
I am not familiar with the association of Babesia with specific immune deficiency. I am not sure how to interpret the Babesia FISH test in your husband’s setting.
Hi;
Was diagnosed with WA1,
I have used a combination of Mepron and Zithromax for 2 months and Malarone with Zithromax for another 4 weeks. Took Coartem for three days.
While the burning and some aches has subsided quite a bit, I started getting sever air hunger, which I initially did not have at all. I also do not have any night or day sweats. The test showed that the B. Duncani AB jumped from 1:256 to 1:512.
Anything else you would try? Can air hunger be a bartonella or Borellia symptom?
I also try a combination of clindamycin and quinine in my patients if needed. I do not feel we understand air hunger all that well. I always look for coinfections. I also look for other medical problems.
Have you seen Air Hunger with bartonella or Borellia?
We do not have a test to measure air hunger in individuals with Babesia let alone other tick-borne infections.
Everyone in my Lyme group that has Babesia describes air hunger. I myself had Babesia and experienced episodes of air hunger. It seems to be a defining symptom of Babesia!!!
I have this symptom for 3 months now! I had some night sweats a few times. I’m mildly anemic 10.5. This symptom won’t go away for me. I eat healthy but I can’t get rid of it. I have fatigue at times. My symptoms started in Mid April it was my stomach at first I didn’t have an appetite then I lost a lost of weight. Everything else got better I’m eating but then I developed this air hunger that won’t go away. Every dr I’ve seen are like my lungs are good my X-rays are good. My oxygen is normal. I just want to breathe. I started taking irons pills recently and my vitamin d pills!
I have seen Babesia patients with air hunger and sweats. They often have other symptoms including fatigue and stomach issues. I advise my patients to include a consultation with a doctor experienced in working with Lyme disease.
My triglycerides jumped from 128 to 687 in just a few months since being diagnosed with Babesia, are these two related, or the malarone medication? Is this common?
There are too many reasons for an elevated triglyceride reading to come to any conclusions.
Hello, I had an igenex test done for babesia Lyme and Bart. Babesia microti and duncani came back positive for active infection. And Lyme was equivocal igm 24, 41 and 39. Is this accurate enough to say I have babesia and Lyme. I have alll the symptoms except sweats. I’m 22 and suffering bad for 3 years now !
The tests can be supportive. Your doctor will still have to use clinical judgment.
My #1 symptom is I am off balance when I walk, it has destroyed my life for 3 yrs and at every appt with my LLMD we discuss it is not improving and I am confused if it is a Babesia or Bart symptom and have asked my LLMD previously but I dont think he ever really answered me. I have been treating bart for over 9 mo and balance not improving . Dr. Burrascano list “off balance; tipsy feeling” as a Babesia symptom and the checklist I complete at every LLMD appt also list off balance as a Babesia symptom. Can someone please clarify for me?
Can you please tell me if the feeling of off balance is a Babesia symptom? This is my worst symptom and I am currently treating with Azithromycine, Malorone & Bactrim DS.
The autonomic nervous system is often the cause of balance issues in my patients. I am not sure which tick-borne illness is behind the balance issues. I also advise a neurologist and/or ENT if appropriate.
I have a positive IFA igg babesia duncani test from quest. 1:256. Negative babesia FISH from igenx. Previously postive WB IGG through labcorp for Lyme with 5 bands. I definitely had tickborne disease exposure. But, I have been sick for about a year. I think the Lyme is dead, following 7 months of antibiotics. However, I still have night sweats, muscle aches, headaches, brain fog. I have seen a multitude of specialists and ruled out neuro, autoimmune type causes. Including by lumbar puncture and MRI.
Given the recent babesia IFA and symptoms…. could I have duncani even after a year since tick bite?
Thanks!
I have patients with unresolved issues including Babesia. Babesia Duncani can be difficult to treat You may want to have a second doctor look over your treatment to see if there are any other options.
Hello Dr. Cameron, I was diagnosed with Babesia Duncani serum IgM 80 on a test from IGenex. What would be the best bet treatment?
Most of the research focuses on Babesia microti. I start with atovaquone. I also look for other co-infections.
Because Lyme is so common, doctors often assume it is the sole problem in patients with tickborne infection, not recognizing newer diseases, says Durham’s doctor, Daniel J. Cameron, M.D., an internist and epidemiologist in Mount Kisco, New York, and past president of the International Lyme and Associated Diseases Society. It’s possible that undetected coinfections could help explain the medical mystery that is known as category 4, or “chronic,” Lyme. Some sufferers contend their symptoms continue to affect them after the standard treatment of two to four weeks, but not all doctors believe Lyme persists. What if some of these patients continue to struggle because they have another tick-borne infection? “You have to examine whether you have prescribed appropriate antibiotics for each infection that might have been in that tick,” Dr. Cameron says. “The problem is that doctors are reluctant to treat any more than the bare minimum, and they lose the opportunity to treat people in a timely manner.”
Diagnosed with Babesia, being treated for many months with Atovaquone and other abx.
Have you ever seen muscle wasting in lyme or its co-infections? I feel like I have muscle wasting in left upper arm.
There can be several reasons. One could be a frozen shoulder. The frozen shoulder might be related to pain from a tick borne illness. Several doctors will have to weigh in.
Is frozen shoulder from Lyme/Babesia something that you see frequently? I thought that my shoulder ‘injury’ was overuse – even though that diagnosis never really felt correct in my heart….regardless, it refuses to get better, ive done nearly every form of PT – in august it will be 2 painful/sad years. MRI’s have been inconclusive, as shoulder MRI’s often are. Coincidentally After nearly 2 years of Many other (typical Lyme) symptoms that I had determined must have been brought on by Stress, a long string of Dr. visits and several different medications for a disgusting ‘rash’ on my face – May 1st 2020, I was on day 6 of what we now know was a bad Herx – the Dr in the local Hospital ED, who was ironically the 1st Dr I saw 5 months prior for my face, quickly ruled out Covid and based on our conversations both then & in January ordered a Lyme Test and immediately started me on Doxycycline.
sorry, Long Story – but, OMG Frozen Shoulder & Lyme/Babesia? is there a way for me to figure out if this is the cause of my shoulder issues?
many thanks in advance.
i am not yet sure if I am positive for Babesia- but my Dr mentioned that we should think about having me tested …
I have seen patients in my practice with Lyme disease and co-infections which act like a frozen shoulder. They typically have other issues as in your case. I often involve an orthopedist and PT along with antibiotics. Call my office at 914 666 4665 if you have any questions.
Hi;
Have you have any recent success stories treating B. Duncani?
Yes
I was diagnosed with Lyme and babesia in 1995. I was treated for Lyme disease, but not the babesia. Fast forward to 2017 and I was diagnosed with retinopathy and am losing my vision. I have suffered from the initial symptoms for 25 years. After going to multiple doctors, I lost hope of ever being symptom-free. However, I saw a video of Dr. Richard Horowitz https://www.youtube.com/watch?v=O9a-2Nb2sbk&t=2784s speaking at a physician’s symposium and started a journey of looking into babesia. I tested positive for an active infection two months ago. However, I have been denied by 2 infectious disease specialists in northern California. I am wondering if you could recommend a medical group or doctor who can help treat me.
Thank you for your time.
You could contact LymeDisease.org or ILADS.org. You could also call my office in New York at 914 666 4665 for a telemedicine appointment.
My wife is being treated for chronic lyme along with babesia duncani. She recently was tested for Bartonella which came back negative (fortunately). She has been taking low dose disulfiram since other treatments have not been effective, however, we believe that the babesia symptoms are most prominent and not addressed by disulfiram. Her doctor has suggested an anti-malarial such as plaquenil to treat the babesia. (She cannot take mepron and disulfiram simultaneously since there is alcohol in mepron). Are you aware of plaquenil being effective with babesia duncani? Are there any other anti-malarial medications to consider?
I am not sure Plaquenil is effective for treatment. I have used a combination of clindamycin and quinine but there are more side effects. I might suggest checking out whether Malarone which includes the active medication in Mepron has any alcohol.
Hi,
I was treated 10 plus years ago actually by Dr. Cameron for Lyme Disease with PICC placement and intravenous antibiotics with ceftriaxone. My main symptoms of Lyme at that time were joint pain, effusion and fatigue. Unfortunately my symptoms have returned. To my knowledge, I am not sure if I had babesia.Wish there were more reliable tests to check for this. My Western Blot came back last month with two bands (41kd and 58kd IGG). This is considered a normal result and my doctors will not treatment despite my testing always been equivocal previously. I live in Florida right now so I am having trouble finding a Lyme Specialst down here for a second opinion. I have a bakers cyst on my MRI of one of my knees which I suppose could have formed due to all of the fluid. I am planning to have that drained and if my symtoms still do not resolve, follow up with Dr. Cameron again. Of course I am being sent to Rheumatology like I was last time and recommended to start immunosuppressive medications for treatment of RA all on the basis of my ANA being elevated and my synovial fluid showing some inflammation, even though my CRP, EST, RF, CCP and DS DNA for lupus are all negative.
Sorry to hear your symptoms are back. Call my office at 914-666-4665 for a telemedicine evaluation if you stay ill.
Hello, my 4 year old daughter had an engorged deer tick above her right ear that we sent in for testing to tick check. It came back positive for babesia microti. We had her on one month of amoxicillin tight after tick bite. Right after we got off of amoxicillin she developed large sore and swollen lymph nodes along the back of her neck, with the node on the right side of her neck closest to the tick bite being twice the size of the others. She complained of pain when moving her neck and would not let us palpate the nodes. We went for blood test, which came back negative for babesia microti, but I am suspicious given the difficulty of dx in humans. The nodes have since gone down but are still present. I just want to make sure this isn’t something that will affect her long term. She is healthy enough, but my daughter was born prematurely and spent the first month of her life in the NICU due to respiratory issues. I feel like her lungs and system are a little more vulnerable than typical. How does one treat this in a 4yo? Are the drugs safe for this age? Should I see an infectious disease specialist? I just feel like no one will treat this given that her blood test came back negative, even though the tick tested positive And she has symptoms.
I understand your concern with Babesia. Amoxicillin does not treat Babesia. It can be difficult to determine if Babesia in the tick was transmitted. There is a pediatric dose of Malarone available. I would include a doctor with experience in taking care of young children with tick-borne illnesses.
Hello,
I got infected 25days ago ( tick in leg for two days at least) and few days later symptoms started. Been on Doxycycline for 20 days and still heavy joints pain, fatigue and various spots pain.
When can I start testing for co-infections and which ones should I do ( I live in Europe)
Many thanks
Nick
I typically recommend followup with a doctor experienced in treating Lyme disease to include checking for co-infections. I also recommend seeing a primary to make sure there is not another illness.
Thanks doctor.
Results came positive for Chlamydia Pneumoniae and Bartonella henselae, Lyme slightly positive ( been tested after 2 weeks on Doxy). Other bacterias not tested yet. After 25 days on Doxy still have joints pain and fatigue. What would you recommend?
Thank you.
Great question. I find I need to individualize treatment for my patients. You will need to followup with your doctor. Call my office at 914 666 4665 if you have any questions.
Hello, thank you for this article. After one weeks of extreme fatigue, muscle weakness, loss of appetite and rapid afib I thought would go away, mt dr insisted I go to the ER for a cardiac eval. I was in rapid afib around 180 and given infusions to stabalize my heart. I am a healthy 64 year old female living in mass. Blood work in hospital showed lowed white blood, sodium and I think an increase in liver enzymes. My skin and eyes were also yellow and blood ptessure extremely low.Er doc asked if I found any tick bite, I said no but I live near a wooded area. Three days later tests showed babesia. I was immediately put on a low dose of heart med for the afib, 500mg of azithromycin once a day and 750mg/5ml liquid atovaquone twice a day. It has been one week and I am starting to feel like myself again. My blood and other tests will be redone in three to four weeks. I am grateful for what I think was an early diagnosis. More awareness is needed for this tick illness that should not be left untreated. A neighbor also had it 5 years ago and almost died of kidney failure. She waited too long.Insist and find good doctors like Dr Cameron.
Thank you for sharing your story. I treat my patients with Babesia longer than the 10 days course. Call my office at 914 666 4665 if you have any questions.
Hi Dr. Cameron,
I am going to begin treatment for babesia and chronic lyme. I am 38yo and have rarely taken antibiotics. I will be taking azithromycin and atovaquone. My babesia test came back negative. Have you rx in scenarios like this? Should I worry about herx side effects?
I have treated patients with Babesia using clinical judgment if the tests are negative. I typically do not find a 10-day course of azithromycin and atovaquone sufficient. I have seen Herxheimer reactions in some patients some of the time. Call my office at 914-666 4665 if you have any questions.
Hi Dr Cameron,
I have just finished a course of doxycycline for a tick bite and the dr called with bloodwork results. He reported that one test was negative for Lyme, one was borderline positive and one was positive for Babesiosis. He said to call if I become sick with fever, aches, chills, sweats in the next few weeks. I was sick with pain, sweats and extreme fatigue when I was initially was diagnosed but improved with the doxy and feel ok now 3 weeks later except for fatigue. Should I be treated for the Babesiosis to be on the safe side? I am concerned and do not want to wait to get sick like that again or have serious heart, lung or organ issues if I wait. I already have mild asthma and Epstein Barr. Thank you.
I find Babesia symptoms become less severe without treatment. I often see symptoms reemerge. I often find Babesia to be the answer for someone chronically ill.
I discussed sweats in a blog at https://danielcameronmd.com/sweats-may-be-a-sign-of-babesia/ Sweats appear to be caused by other tick borne infections.
I often treat my patients with symptoms, sweats and a positive test for Babesia. Call my office at 914 666 4665 if you have any questions.
Hi Dr. Cameron,
I was diagnosed this week with babesia. Started on Zpak and Atovaquone for 10 days. I presented with fever, sweats, cough, extreme fatigue, and hip joint pain. After the course of medication should I be re-tested? And if it comes back negative am I cured? Or do they stop treatment based on if I am feeling better. I am concerned about prolonged issues, but obviously will not know if the medications have rid me of this until I see how I feel after I guess?
A 10 day course of treatment was effective at clearing the parasite from the red blood cells if caught early. I have been concerned with the remaining signs and symptoms. I typically treat longer based on clinical judgment. Call my office at 914 666 4665 in New York if you have any questions.
Hi Dr. Cameron. My wife is immunosuppressed due to multiple organ transplant (heart/lung). She was having high fever (102+) and night sweats. Negative on Lyme test, however, positive on B. Microti. Not infected more than 4 weeks as that is how long we have been here in the north. No evidence of vector site. Was told it might be too early for Lyme to show up diagnostically. Rash appeared just as she was starting to take doxycycline as a precaution. Fever and sweats are gone after a few days of doxy, It seems to be understood by the Tx M.D. that the doxy will take care of the Lyme if it was indeed present. 1). Is B. Microti ALWAYS a co-infection? Also, she was just prescribed atovaqune (liquid)/azithromycin combo by the transplant team for 10 days. 2). Is 10 days long enough to treat b. microti? My online research seems to suggest otherwise and that a 3-4 month treatment would be more appropriate. Would you be clinically available for further consultation on treatment and testing if necessary while we are up here? Thanks for all the information on your website. It has been very helpful.
Sweats can happen in Lyme disease in some cases. I am glad their treatment includes medications for Babesia. I have often had to treat Babesia longer to get a good outcome. Call my office at 914 666 4665 as we are available.
Igenex labs… Babesia duncani IFA.. IgM 40 and Babesia duncani IFA.. IgG <40
Bartonella vinsonii serum IgM positive…spp(genus) positive………Bartonella vinsonii IgG serum negative
LLMAD started me on 500mg Azthromycin only(single drug regimen) for Bartonella… on for 12 days then off for 2…then on for 5 days and off for 2 for preceding weeks. Days 4 through 7 I had some shortness of breath (home pulse ox was still always in the mid to upper 90s) and feeling not so good.
I contacted LLMD for some herxing advice….they want me to take a day off …but tomorrow change plans to start treating Babesia first instead of Bartonell first (not sure of approach yet).
Isn't this a little atypical….it looks to me that you want to treat Bartonella first and treat with a 2 drug protocol when you do.
I have no been on the Azthromycin for 7 days…..not sure what to do
Thanks much
I can’t comment on your case without an evaluation. I typically make sure my initial treatment addresses Babesia instead of solely addressing Bartonella. Call my office at 914 666 4665 if you have any questions.
I tested positive using IGeneX with Lyme, and 7 other co-infections in 2017. I got sick with all of the symptoms of Lyme disease after visiting the mountains of NC for a week 23 years ago. No EM. At the time, I tested negative for Lyme and my doctor would not treat me for Lyme until 4 months later. I was given 14 days of doxycycline. Within 2 days, my symptoms began to disappear. Then the myalgia started. Diagnosed with Fibromyalgia. Fast Forward, I tested positive for Babesia FISH in Nov 2019. I have not been treated with this since I was having some serious GI problems. GI problem is mostly resolved. I am in Florida and have seen so many doctors for one symptom or another. I am being affected in my CNS, neurological, extreme fatigue, headaches, blurred vision at times, etc. I have gone to a Lyme doctor but can’t treat me other than with oral medications. Doctors in Florida I have visited do not believe or treat tick borne infections. Any recommendations?
It can be difficult to find a doctor with experience treating Lyme disease. You might find a doctor by checking out websites e.g., Global Lyme Alliance, the Lyme Disease Association and ILADS.
It’s the worst it took over 4yrs to finally be a little hopeful – I’ve been to every dr. With same symptoms -I also live in Florida I just now have an Infectious Disease Dr. that is listening to me-she sent me for bloodwork that I’ve been trying to get tested for years now that all came back positive for Lyme as well as Toxoplasmosis go figure as I can’t even picture getting off the couch so tired always-4yrs later anyways she put me on Doxycycline and another antibiotic and sent me for bloodwork waiting to see the results of exactly what and how she plans on treating me I have my next appointment September 3rd ♀️
Hi Dr. Daniel! I was bit by a tick a month ago and was put on a 21 day course of doxy (100mg twice a day). I had the EM rash (not at location of tick bite) and random rashes that keep coming and go on my knees, and muscle pain in my lower legs. I have 4 days left of the doxy and my muscle pains in legs still didn’t go away. Is 21 days enough? Or do I need more?
Thanks!
I have my patients return for follow-up before ending treatment. I have had to extend treatment or change treatment if the symptoms remain. Some doctors do not extend treatment. Call my office at 914 666 4665 if you have any questions.
Hi Dr. Cameron,
I have been looking all over the net since my husband was diagnosed with Babesiosis. It is believed that it was caught early with a low level of parasite in his blood. He had drenching sweats, up and down fevers for two weeks, until the fevers reached 100+ and peaked at 103. We went to ER and they hospitalized him for one night and he was then put on a week of Azithromycin and Atovaquone, along with Doxycycline just in case he had lyme. Lyme came back negative and after about 4 days he started to feel better, no fevers, sweats and his appetite returned. We went for a follow up with the current doctor assigned and she retested his blood and it came back negative for Babesiosis, she gave him three more days of meds, 10 days total. Should we assume he is healed now? Or should we insist on another blood test to ensure they are gone? The blood test taken 8 days after initial diagnosis came back normal. Thank you so much!!
Babesia treatment is most effective if patients are sick enough to be diagnosed quickly. I typically treat longer if there are persistant symptoms. I don’t continue treatment if my patients are well. Instead, I follow them.
Hi. Is positive igg mean I still have Lyme ?
A positive IgG in viral infection generally means the infection is resolving. A positive IgG for HIV does not mean the infection is over. A positive IgG for Lyme disease means exposure. It does not tell whether the infection has cleared. Call my office at 914 666 4665 if you have any questions.
hi Dr Cameron,
i am positive for babesia microti IgM
and positive for borrelia IgG
i work w a naturopath here but i wanted a second option.
i want to try the atovaquone for the babesia but not sure which antibiotic to try in combination for the borrelia?
secondly, how many milligrams and days do you recommend for the atovaquone and the antibiotic?
lastly, why would you need an antibiotic for babesia by itself if it’s a parasite and not a bacteria?
Dr. Cameron, Please provide references or links to any info regarding the use of TINIDAZOLE or FLAGYL (metronidazole) for Babesiosis. My husband’s MD (non-LLMD) is willing to prescribe but would appreciate direction & documentation.
2 years ago my husband was diagnosed with Babesia duncani (IgM 640 with positive FISH) & then Lyme. Multiple ANTIBIOTIC regimes x 11 months – no lasting benefit. 8 months ANTABUSE (Disulfiram) – ineffective.
We can’t pinpoint the onset of the Babesia & Lyme, tho he’s been treated for similar symptoms (possibly misdiagnosed Babesia?) for years: 1) Severe FLU episodes x 48 years, sometimes responding well to TETRACYCLINE/DOXYCYCLINE. 2) A fatigue/fibromyalgia-type syndrome x 31 years. 3) Presumptive Giardiasis episodes x 32 years that responded dramatically at times to PRN-use of FLAGYL. 4) Chronic anemia without GI pathology.
If treatment with either TINIDAZOLE or FLAGYL could treat the Babesia, it would be life-saving. My husband feels he can’t continue on with his severe generalized pain, weakness, dizziness, chills, sweats, headaches, etc.
I have not seen any published literature to support the use of Tinidazole or Flagyl for Babesia. I have had some success in my practice but I was not sure if the problem was Babesia. We typically do not see any support for antibiotics that are generic.
Thanks for your kind reply. Would you share the dosages you’ve used, please?
I have had to individualize treatment.
Thanks you. Final question. In your experience could his long-standing symptoms described above have been Babesia/Lyme all along? At least the chronic fatige/fibromyalgia-type symptoms which have progressed x 31 years? Thanks, again.
I have seen it.
My then 7 yo was bit by a tick but no symptoms developed immediately, and she eventually tested neg for Lyme via western blot. She also had what looked like the worst flu of her little life that year.
Within that year she started losing muscle tone in her hands, and now at 11 she has progressive axonal neuropathy in all four extremities. In the last 8 mo she has lost 20 lbs of muscle and is having autoimmune neuropathy teased out, one of the two differentials being Sjrogrens neuropathy or Chronic Guillan Barré Syndrome (aka CIDP). She is starting IVIG therapy asap, since the wasting was just discovered (drs kept saying it was fat-loss).
Because the year her symptoms started she had the flu and was also but by a tick (and she’s bound to have Sjrogrens since dad’s mon and I have it, but not with neuropathy) I’d like to have the tick bite ruled in/out as a probable cause since it could impact treatment.
Is nearly 5 years post-bite too late to check for Babeosis? Would antibodies show historical infection?
Thank you!!
The tick borne infections tests are not as reliable as I would like. I typically test my patients anyway. Some of my patients have more than one issue. I have to treat some of my patients for a tick borne infection using clinical judgement. I also advise my patients to work with their other doctors.
Hello. I appreciate your article. I wanted to ask if you are diagnosed late, meaning years later, does the side effects of these infections tend to worsen? 7 years ago I randomly started getting intermittent foot drop. After my first episode 6 mos. later my thyriod suddenly went compute and I was diagnosed with Hashimotos. 3 years ago my gallbladder became inflamed and wouldnt let bile pass from liver to duodenum, so I got inflammation in my liver, and my gallbladder was removed. Then I lost 27 lbs and my stomach, which I had problems for awhile at that point, started to throw up or not breakdown most foods. So my diet became limited and due to that I lost another 5 to 7 lbs. So I am below my BMI, no matter how much I try to get it higher. My body begin to weaken muscular and neurologically, and my foot drop led to full permanent paralyzation in my left leg, which is now over 3cm smaller in quad then right. Even though my right leg is starting to go as well. I also have blood flow issues, where it is slower then the 3 and down to 1 1/2 in both legs, left lower obviously worse. My legs and feet are always blue despite weather temperature outside or the temperature of my feet. Even though they run cold, but even heated still blue. I have low everything in my blood as in nutrients and minerals, and high inflammatory markers even d dimer, C4,TGF1 beta, etc. Plus high anti prothrombin antibodies, but not antiphoslipid. Just curious because my IGMs for lyme, IGMs for RMSP, and Babesia Duncani levels are high, even after being on my 3rd round of meds – 2mos a round on varies antibotics and antiparasectics. Wondering if in blood long enough does it take a long time to get well. Sorry so long
You are not alone. I typically recommend consultations with a broad range of doctors to rule out other causes. In addition, I have had patients with more than one illness. Finally, I have patients with blue feet due to acrocyanosis, an autonomic disorder.
Hi, thanks for the great information. I pulled a tick off my back a week ago (NY State) and consulted with my PCP; as a result just finished 5 day course of doxycycline 200mg/ day as prophylactic for lyme. Tick lab results came back positive for Borrelia burgdorferi and Babesia microti. Tested specimen: adult female deer tick (Ixodes scapularis), semi-engorged for 36 hours. Would you advise simply waiting for Symptoms or is there a recommended proactive approach with regards to Babesia microti exposure? Thank you.
I would prefer a three week course with a reevaluation for my patients with a semi-engorged tick. The risk of transmission climbs to 20 minutes. Doxycycline does not work for Babesia. There is no consensus for prophylactic treatment for Babesia. I have had to individualize my assessment for each patient.
I see that IDSA released recommendation for Babesia, as for Babesia Duncani, they recommend IV clindamycin plus oral quinine, is this a new recommendation? They say “The efficacy of atovaquone plus azithromycin in treating such infection has not been evaluated”.
Is this a new approach?
IV clindamycin and oral quinine was once the preferred treatment for Babesia. Unfortunately, the combination was associated with a lot of side effects. Krause and colleagues found Zithromax and Mepron to be just as effective without side effects. Most doctor and their patients are more likely to use Zithromax and Mepron. Some doctors still use IV clindamycin and oral quinine.
I was diagnosed and treated for babesia over the early summer. I’m feeling almost as worse as I did in the summer. Is this normal? Could I also have lymes?They never tested me and the babesia was found incidentally.
I have patients in my practice that require longer treatment. I also have patients with another tick borne infection that does not show up on a blood test and respond to treatment.
Dr Cameron,
I was diagnosed with Babesia in June and was given antibiotic and anti malaria drug for ten days . I was bed ridden with complete exhaustion for two weeks. I do suffer from PCOS and have chronic Epstein Barr. I am feeling similar symptoms as in June . Body aches , headaches, exhaustion. I asked my Dr about retesting or another treatment ? She has stated I should be cured after one treatment . Can you offer some advice ?
I have patients in my practice who have benefited from longer treatment for Babesia. Other doctors have published cases where long therapy was effective. I also have to look for other tick borne infections once I find one. Lastly, I advise my patients to consult other specialists to rule out other infections. Call my office at 914 666 4665 if you have any questions.
Daniel, my Dr stopped my babesia treatment after being on for 2 months. Is this sufficient time to kill this infection?
Also he placed me on Tetralysal 300mg 1 daily, cefuroxime 500mg twice daily + zihromax 250mg twice daily for Mondays, Wednesday and Fridays to treat bartonella and lyme. In your opinion is zithromax dose too low and should it not be every day? My recent bloods were out so I don’t know if he prescribed less as a result of this??
I cannot comment on the treatment regimen without your being under may care. I can say that Zithromax stays in the system at decent levels for 5 days so Zithromax 500 every other day is similar to 250 po bid.
Hi Dr. Cameron,
I was treated for lyme in 2017 with a year of oral antibiotics and have still had problems with mold, Candida, EBV, etc. I recently found out via DNA Connexions that I have all 3 strains of babesia and borrelia recurrentis. Are herbals effective? I am concerned about the Candida. Thank you, I really admire your work.
I am sorry to hear you are still ill. I am not sure how reliable the DNA Connexions test until they release tests to validate their results. BTW Babesia can be overlooked. I leave answer regarding Candida and Herbal medications to doctors who practice integrative medicine.
Thank you so much. I may contact your office about a consult
Dear Dr. Cameron,
I am a 38 year old woman who suspected she was bit by a tick about a year and half ago. I had several tests all come back negative for multiple things, but I felt awful this whole year: exhausted, nonstop headaches, joint pain, tons of pressure in my head and this odd feeling of dread, like an ominous presence. I finally was told about a specialty Lyme clinic where they did much broader testing and I found out that I do in fact, have Babesia. The doctor put me on a 6 week course of atovaquone in liquid form and azithromycin. That seemed like a good long course. But after being off the meds for two weeks I was starting to feel bad again, mostly the headaches and the pressure in my head which makes it difficult to think about anything else. She now has me on Malarone in pill form, which I guess I will be taking somewhat indefinitely. So far I still feel lousy and the pills don’t seem to be catching up like the antibiotics did. Do you think I should take more atovquone with the azithromycin? Or do you find that patients who stay on the Malarone long enough (I mean 6 months or something) tend to see things clear up? Thank you! I really feel like I’m going crazy.
I have patients in my practice that have similar concerns. The treatment for Babesia helps but is is hard to wrap it up. I have found changing the Zithromax helps. BTW, I often use Malarone rather than the liquid. I also work with my patients to make sure they do not overlook another illness.
Hi Dr. Cameron,
I had Babesiosis in 1977 when it was extremely rare. I was 27 at the time and spleenectomized. I was hospitalized at Montefiore Hospital in New York. Back then the medical community knew very little. The treatment I received was blood transfusions and Chloroquine. I survived, barely, and have had health issues ever since. I have tremors, RA , EoE and AFib. I believe all of these illnesses can be traced back to Babesiosis. Other Drs. think I am crazy but it seems to me if my blood still carries the disease and is dangerous for others then it is still affecting me. What is your opinion?
I have patients where they do well with other protocols. I would consider treatment if faced with similar presentations to include Mepron or Malarone for Babesia.
Hi Dr. Cameron,
Husband is being treated for Lyme and coinfection‘s currently. This has been an issue for him for the last decade on and off. We seem to get it under control and then there is a sort of relapse. In the past two months, he has developed a symptom where the veins in his hands and arms become so enlarged. He has never had an issue like this before and he also feels pressure when it happens. It has been happening pretty frequently. I have been treated for Lyme and coinfection’s and have never had or heard of this symptom. Is this something that you are familiar with? I cannot find any information about this on any symptom checklist. He has been to the doctor and mentioned it to his Lyme doctor but nobody really has any answers.
Hi Lorena,
I’m reading through these comments and found this interesting as I have the same thing and don’t know anyone else w Lyme that has it. My LLMD isn’t quite sure about the cause and I saw a vascular surgeon who also didn’t know the reason. He thought it was connected to dysautonomia. I’m being treated for Babesia and Bartonella. I’ve had positive tests for both, not Borrelia. I was diagnosed with mild adrenergic sympathetic dysfunction from neurologist. I started antibiotic treatment Nov 2020, my veins began dilating around Feb 2021 and hasn’t improved. It’s better when elevated and during cooler weather, awful in heat and humidity. I’d be interested if your husband has had any improvements.
I have the exact same thing happening. I’ve always had tiny veins, hard to draw blood. Not much in the way of visible veins. Over the past few months all my visible veins are more visible. And I have a quite enlarged vein in my right bicep. I don’t feel pressure though.
If I wack my hand on something, a vein will pop up and I have to ice/compress it.
I’ve had no luck with any doctor, except my lyme doctor, take me seriously. Been to neurologist who dismissed my symptoms as something I “believed”. Saw a cardiologist. No one has any insight.
And then this morning, I get a call from my Lyme doctor. After 12 years and probably half a dozen tests, I finally tested positive for Babesia
I have been having odd blood pressure issues, too high, too low, heart rate to low, too high.
I have the exact same thing happening. I’ve always had tiny veins, hard to draw blood. Not much in the way of visible veins. Over the past few months all my visible veins are more visible. And I have a quite enlarged vein in my right bicep. I don’t feel pressure though.
If I wack my hand on something, a vein will pop up and I have to ice/compress it.
I’ve had no luck with any doctor, except my lyme doctor, take me seriously. Been to neurologist who dismissed my symptoms as something I “believed”. Saw a cardiologist. No one has any insight.
And then this morning, I get a call from my Lyme doctor. After 12 years and probably half a dozen tests, I finally tested positive for Babesia
I have been having odd blood pressure issues, too high, too low, heart rate to low, too high.
Hi Dr. Cameron,
How common is babesia, bartonella & Lyme to get misdiagnosed as Alzheimer’s? Currently going to Dr. Frid in NYC, starting IVIG treatment in 2 weeks to see if my fathers dementia symptoms clear up. He is only 59. Was diagnosed in 2016 with early on set Alzheimer’s
I have patients with Babesia, Bartonella, and Lyme disease with cognitive problems. We could use a study to determine how often these cognitive programs progress to Alzheimer’s disease. I typically start with antibiotic treatment rather than IVIG.
Hi Dan, just had treatment for Babesia 2 months with Malarone. Would running antibodies to Babesia confirm the infection has been killed?
I have not found a negative lab test for Babesia all that helpful in my practice.
My previous test before treatment with Malarone came back positive. Will re-test with a negative mean it is most likely gone? In my individual case, basing treatment success/failure on symptom relief is not possible due to psych meds suppressing symptoms.
I have not found a negative test for Babesia a reliable measure of clearance of the Babesia. You will need to work it out with your doctor.
I have been diagnosed with POTS Syndrome, and CIRS. I am extremely ill. My worse symptoms are the neurological symptoms. They are so severe that I don’t even feel alive. I know CIRS can cause these symptoms as well as Babesia. My doctor had me to take some Bart drops to see if I was going to have an reaction to them. I really didn’t have an herx reaction but it’s it’s also hard to tell with how sick I am. Some of my other symptoms are night sweats, cannot control body temperature, chest pains and burning, having an hard time breathing, stomach pain, the pots symptoms, strong palpitations, headaches, fatigue, muscle weakness, and etc. Can you give me some advice about all this I have going on?
I have patients in my practice who also have autonomic abnormalities.
Dear Dr Cameron,
Im from Europe , treating lyme / bart/ babesia ( igg found in european lab) with lyme doctor. 4 months after tick bite i started treatment with malaron ( 2 pills a day)/ azythro but in a month developed increased heart rate and heavy legs…so we stopped this protocol and focused on bartonella ( rifampicin + azythro) which improved heart rate / heavy legs symptoms but after 3 months increased
heart rate and shortness of breath is back…In your experience malarone / azythro can initially exorcebate babesia symptoms ( herx) or it s a gradual improvement? What is the normal dose for malaron ( i m afraid 2 pills/ day for 50 kg adult is not adequate)Not sure if i should get back to babesia treatment…Thank you so much!
I have patients who thought they were sensitive to the treatment. They end up with the same symptoms of a totally different medication suggesting the flareup is due to the disease and not the treatment. I often start with Malarone 1 po bid to increase the chance my patients will tolerate the drug. I have the option of increasing the dose as Malarone had 250 mg of atovaquone and Mepron has atovaquone.
Hi Dr Cameron,
I have had epigastric pain since Dec; gone through so many gastro tests and nothing shows up. Even had my gallbladder removed as they thought it was the culprit. Originally I was constantly nauseous, slight fever, trip to the ER showed nothing.
Finally this past week I saw an urgent care doctor as my Ribs are in awful pain like costochondritis, mainly in the sternum, still upper stomach pain, brain fog, some back pain, and it hurts to wear a bra, and terrible anxiety from all of this. I asked for a lymes test (I’ve asked other drs who all told me I didn’t have any of the symptoms), and found out on Sunday that the panel for Babesia came back positive. Started me on 10 days of azith and atovaquone twice a day.
Have you had patients with the rib/stomach pains like mine, and have the resolved once treated? Will it likely take longer to resolve/more meds due to the length of time that this has been going on? Appreciate any advice, I’m very nervous that this won’t go away, but happy to have likely finally found the culprit. The stomach/rib pain can be really tough, and has gotten worse since starting the meds 2 days ago (maybe herxing?) Seeing an ID Dr on Thursday, but may want a telehealth with you if I’m not comfortable with their knowledge. I’m in NJ.
Thank you for your time,
Steph
I often find ill defined stomach problems in my patients with tick borne illnesses, likely due autonomic issues. I typically find other issues beyond the stomach that help with the diagnosis. I have not found 10 days of treatment as helpful as I would like particularly if my patient has been ill for a while. I have also been concerned that another tick borne illness might be present but not identified. I also want to make sure there is no other illness. All the best with your ID specialist.
Hi Dr.Cameron,
My little girl was bit by a tick and contracted Babesia from it. She will be 2 in October 2021. She was symptomatic right away, she was clingy, tired wanted to nap often, and poor appetite. She was treated for 10 days, with two medications. Symptoms improved, but now more than a month later she was developed lose/soft stools, not quite diarrhea but pretty close. She is clingy again, tired and asking to nap and her appetite is poor. I am worried that the Babesia has not cleared. Looking for any additional information on treatment on such young children.
I have Lyme disease patients with Babesia who have done well with longer treatment. I do not take care of children that age. You might contact Global Lyme Alliance, the Lyme Disease Association or ILADS for suggestions.
Why can’t you see a toddler ?
I don’t have experience treating toddlers. sorry.
What is the upper limit for Malarone per day? I have take Mepron in the past 2 tbspn twice daily & switched to Malarone for insurance coverage. Malarone has much less atovaquone per tablet, so what is the upper limit per day.
You have to work with your doctor to determine the best dosage for you. One tsp. of Mepron has 750 mg of atovaquone. One Malarone has 250 mg of atovaquone and 100 mg of proguanil.
Have you treated patients with more than two malarone tablets per day?
yes
Im a 50kg / 100lbs 44y male with babesia.
Many llmd prescribe malarone 250/100 2pills x day
My doc (after i asked him to take into account my very low weight) is giving me 1 pill a day + 250mg azithro a day
In you experience does this mean treatment should be done longer till remission, and would you advise 1 or 2
pills a day of malarone combined with 250mg or 500mg azythro for anorexic adults?
Some doctors only treat Babesia for 10 days and then only if they see Babesia in the red cells under a microscope. I have had to individualize treatment based on tolerability and efficacy. I have used Mepron that contains 750 mg atovaquone and Malarone that contains 260 atovaquone. I have also used the pediatric dose of 62.5 mg atovaquone depending on tolerability and cost. I typically would rather take Malarone 1/2 po twice a day rather than one a day. I treat based on response to antibiotics. I also look for other causes of the illness.
My son is 20, was diagnosed with babesia 3.5 years ago, has tried all the meds you mention plus DSF and is now on ivermectin. Constant nausea, stomachaches and headaches persist and prevent him from living any kind of normal life. He is his doctor’s most challenging case. Have you ever seen a blood transfusion cure babesiosis? Is there any hope for my son?
I have no experience with transfusions for treatment of Babesia. I have challenging cases in my practice. I also have to make sure I don’t miss another illness.
Are there any new cures for B. Duncani in the pipe line, other than Atovaquone?
A combination of clindamycin and quinine had been used but has been associated with more side effects. There are no other treatment in the pipeline that I am aware of. There are alternative medicine treatments that have been proposed.
Hi Dr Cameron,
I was tested positive for Lyme disease and other viruses and treated with doxycycline for 30 days.
I was also tested positive for Babesiosis and received atovaquone plus azithromycin I believe and was retested negative after three weeks.
It’s been 3 weeks that I stopped the medication and I still have bone pain specially at night in all different parts of my body, I have to lay down every few hours and take a 1-3 hours rest, I often fall asleep. I get head aches when I don’t rest enough like half of the day, and I am so tired. I can’t go to work.
I was tested and I had a bit low potassium levels otherwise my blood is OK. I have this cough since I got infected that worries me. My doctor sent me for X-ray to exclude lung cancer. She doesn’t seem to acknowledge the connection I feel between my cough, my complaint of shortness of breaths and between Babesiosis.. She didn’t reacted about my shortness of breath and cough. I tried to bring it up and each time she ignored it. Earlier I had Lyme without Babesiosis and I didn’t had this strange cough and shortness of breath and this much of migraines and persisting luck of energy. After treatment still I was fine as before. Now at keeps lingering around. I can’t go to work and can’t get unemployment benefits, they don’t give when it is due to to sickness. Can you please advice me if you have similar cases you know of, would you tell your experience please what do they do, and how do you continue with their rehabilitation? What shall I say to my doctor that she start to work with me, I am somehow scared to go back to her and say that I still have my symptoms for fear for not to be taken seriously. Too many questions, sorry, thank you for your article Dr Cameron, it was very comforting to read it.
I have patients in my practice who remain ill despite their initial treatment. The parasites in the red cells typically clear quickly. I have had to retreat some of my patients. I also have to rely on specialists to rule out other causes.
Hi Dr. Cameron,
I got very sick almost 10 years ago and after several weeks was diagnosed with Lyme carditis, hospitalized, and treated with ceftriaxone. I also tested equivocal for babesia but was unable to get treatment for over a year, despite being clearly symptomatic. My symptoms improved with treatment (long story, took several years, 9 docs, and IM bicillin to get my life back) however a year after my initial illness I developed three symptoms that still persist: pain in my hands and feet that worsens with sleep, swollen lymph nodes in my neck (that doctor’s don’t see as problematic but are painful), and spinal pain especially in my sacrum. Hoping you may have helpful insights.
I have patients in my practice where Lyme disease can mimic other issues or exacerbate other issues.
Hi Dr. Cameron,
I got very sick almost 10 years ago and after several weeks was diagnosed with Lyme carditis, hospitalized, and treated with ceftriaxone. I also tested equivocal for babesia but was unable to get treatment for over a year, despite being clearly symptomatic. My symptoms improved with treatment (long story, took several years, 9 docs, and IM bicillin to get my life back) however a year after my initial illness I developed three symptoms that still persist: pain in my hands and feet that worsens with sleep, swollen lymph nodes in my neck (that doctor’s don’t see as problematic but are painful), and spinal pain especially in my sacrum. Hoping you may have helpful insights.
Sounds like symptoms of Cytokine Storm Syndrome outlined here. https://www.verywellhealth.com/cytokine-storm-syndrome-4842383#toc-cytokine-storm-syndrome-symptoms
Sometimes people who experience this refer to it as herxing, as in a herxeimer reaction. Dr. Horowitz explains that herxing and cytokine storm are two ways to describe the same thing going on with the immune system. I thought you might find this information useful. I wish you well.
If the tick that was embedded on me tested positive for Babesia Microti what should I do next? Should I seek treatment, or wait to be tested. It’s been a 8 days. Do I have to wait for symptoms??
I am never sure which infection is transmitted from a tick. I have to make a clinical judgement for each case.
I am never sure which infection is transmitted from a tick. I have to make a clinical judgement for each case.
If the tick that was embedded on me tested positive for Babesia Microti what should I do next? Should I seek treatment, or wait to be tested. It’s been a 8 days. Do I have to wait for symptoms??
Hello,
Can Babesia or Lyme cause severe dysphagia? I’ve developed swallowing issues and have tested positive for both Babesia and Lyme. I’m assuming that these infections can cause autonomic dysfunction – a few years ago I struggled with tachycardia but this improved after treatment.
I advise my patients to work closely with specialists to be sure there is not another cause. I have had Lyme disease patients in my practice who have illnessed cleared that they were not expecdin. Yes, Lyme disease can lead to autonomic dysfuntion.
Hello,
Can Babesia or Lyme cause severe dysphagia? I’ve developed swallowing issues and have tested positive for both Babesia and Lyme. I’m assuming that these infections can cause autonomic dysfunction – a few years ago I struggled with tachycardia but this improved after treatment.
Hi Dr. Cameron,
I live in the southern CT river valley area (about 20 miles north of Lyme) and last month was bitten by a deer tick that tested positive for babesiosis. (It was likely attached for over 36 hrs.) I have noticed symptoms, such as mysterious bruising on my face upon waking, fatigue, GI issues, aches and pains, but have had no hallmark temp my GPs trust as their main indicator of infection. I’m online doing research in preparation for a blood test this afternoon, so I know what to expect. Based on what I’ve gleaned so far, it seems to me that the accepted gold standards don’t seem to be sufficient in diagnosing and treating this (and other) vector borne diseases. Is there a medical professional in my state you can recommend who can help me with testing, diagnosis and treatment?
TIA
Jenn W.
Hi Dr. Cameron,
I was infected somehow early March 2018. Noticed symptoms in days and by 3rd week of June I could barely walk, breath, was so weak I just cried. In middle of divorce so no doctor till November. They sent me straight to hospital for 4 blood transfusions & 2 iron. My hemoglobin was 4.5 and was 12.5 less than a year before. All Lyme tests we negative. I just recently tested positive for 58kdIgG and negative for Babesia. I have always suspected Hemolytic Anemia from my research, and all other tests ruled out any other forms of blood loss.
My question is: IF IN FACT I did have hemolytic anemia, would the parasites be dormant now, and could I end up with this again? I have a PM & R who finally believes me and has started me on Doxycycline & Clarithromycin 30 days ago and I am already noticing lots of things disappearing. I realize this is not the treatment for Babesiosis though. I am curious on your thoughts and if you would also treat for Babesia from what I have shared. I went from 95% healthy to almost dead and have had every problem known to an appear over the past 3 yrs.
Thank you so much,
Kim
There are so many causes of hemolytic anemia for a hematologist to consider. You may never know the cause of the anemia. My patients with Babesia typically do not have a documented history of Babesia.
I was treated for Lyme and co-infections some years ago and when treated for Babesia developed classic night sweats. Periodically those return and I try another treatment for Babesia (think I’ve tried all pharmaceuticals and herbals) and they resolve for another 4-6 months then return. Throughout this time, I have had classic migraines (about 2 every 3 weeks and sometimes 3 day clusters – no prior history). Although Alinia isn’t supposed to treat Babesia, I did a month long course (500 mg once/day) last September and not only have the night sweats gone, but so have the migraine headaches (4 months now – the longest I have gone without a migraine in 15 years). Any thoughts on a possible connection?
I am not sure the connection. I am Alinia worked for you.
Dear Dr. Cameron:
Thank you for taking the time to respond. I have chronic Lyme and the three B coinfections. I also don’t have a spleen, so my integrative doctor prescribed two, 20-day rounds of Atovaquone and Azythromicin to battle Babesia. My main symptoms are fatigue, insomnia and breathlessness if I do just a bit of activity. If I do chores, I get breathless. I will sit down, and it passes, but it definitely affects my quality of life. Do you think the 40 days will be enough to get some relief from the air hunger?
Hello Dr. Cameron, I am infected with borrelia burgdorferi, babesia, and bartonella. I have joint pain, neurologic and psychiatric symptoms. My igenex test also shows 29 for rheumatoid factors, i’m not sure if that is related. I am wondering what is the best antibiotic treatment you recommend. I have bloody diarrhea when taking azithromycin.
In my research I have found what is called triple antibiotic treatment. I am now taking the azithromycin with doxycycline and together it negated the adverse reaction of mono azithromycin treatment. I also take Cefdinir twice a day. With this triple treatment I have seen improvement. No more consistent eye, stomach, and head pain. Feeling less foggy and less irritable. I’m not hearing anymore sounds that aren’t actually there or the ringing in the ears. However I still have great joint pain. Thinking maybe rheumatoid arthritis?
You should try Serrepeptase and digestive enzymes at every meal. It really helps with joint pain.
Greetings Dr Cameron,
I have been sick for 12 years following a tick bite, a stones throw from NY state. being in Canada, the acknowledgement of Lyme and associated infections is ignored and the ignorance in general is profoundly unbelievable and heartbreaking, even amongst infections disease specialists. For most of these 12 years I have been extremely sick. I have no quality of life at all. I am completely house bound, crippled from neuropathic symptoms and disfunction ( no use of my hands and arms) these symptoms and about 40 others are literally killing me. I have one Dr. An environmental Dr who understands and is certain that I have lyme, likely babesiosis and likely more infections. Testing in this country is truly inadequate, and this Dr is limited without hospital privileges. I was on 3 antibiotics for a year, very minimally helpful. I made enough noise to finally get plasma exchange tried, this was more helpful than anything else ever tried but the small but valuable improvements last only a few days, no sustainable or cumulative effects. I am now on Malerone but whether it is side effects or herxing , it is intolerable. My question……. how about Red blood cell exchange to remove the parasite infestation from the blood cells? I can’t find much about it being used for this but it is done in some places, Mexico for one. I can’t get a hematologist to even try it despite my willingness to sign a release, I’m aware of the rare possible risks but I have NOTHING left to loose. The hematologist told me I would get a red blood cell exchange if I was comatose hospitalized and 48 hours from death, I enquired if I should lay around and suffer until then to which I received a shoulder shrug. This is just one small sample of the type of treatment I’ve received for years. I am at a complete loss as to what to do, feeling out of options and time.
Any thoughts or insights would be greatly appreciated
Thank you so much
Red blood exchanges have been helpful in early Babesia when there are parasites still visible in the red blood cells. I don’t have any experience to share about the role of red blood exchanges when Babesia has been present for weeks to months without visible parasites.
Hi Dr. Cameron, I am a 64 year old Cape Cod MA resident who was diagnosed with Lyme/Babesia in June, 2021 (about 9 months ago) after experienced significant sweats, chills and fever. I started the treatment about 6 weeks after contraction as the bite in right thigh did not present as a bulls eye. I was treated with 21 days of doxy, Azithromycin and something for the lungs. I recovered well however continue to have issues with arrhythmia (I get shortness of breath) and nerve issues in my right leg. The leg is weak and gives out after sitting/being at rest and then called on to perform (walk). Any thoughts on how I might be able to address these issues? I have seen a cardiologist about the shortness of breath and will have a nerve test on the right leg. That said, I am wondering if a regime of anti-biotics or herbal treatments might make some sense. The weakness in my right leg is pronounced and somewhat debilitating. Thank you for your time. George Mandt
I refer my patients to cardiologist for shortness of breath. I have often seen air hunger in my patients with Babesia. I have found Malarone or Mepron helpful in my patients with the same presentation.
Hi Dr Cameron.–I am going on over 10 years with Lyme and Babesia and although most of my symptoms have subsided ..it is the air hunger believed to be caused by Babesia that lingers. Is it possible to get my air back after not having it for so long -if so how long of a treatment do you believe it will take 2 months… 6 months or a year or years on antibiotics to get it back? Is it possible to get my air back again after so long and after a long treatment of antibiotics if I choose that route. Will I just get my air back or will I just never be able to breath naturally again. My lung doctor is treating me but that is only to medicate my lungs to breath rather then fixing the problem?
Good questions. I wish I had the answer. There is no test to objectively measure level of air hunger.
Hello Dr Cameron, I have had Lyme disease, the bullseye rash in 1999, was treated with 3 weeks of amoxicillin and never experienced any of the traditional lyme symptoms. I have recently been tested three times this year and only positive for the Babesia via the IGEnIX FISH. Everything else was negative except for IGG of 2 Lyme bands. They were slightly different than the bands found in 2019. Babesia has always been negative.
Well, I have also been infected with mycotoxins and pesticides and CO, other chemicals. If I don’t have traditional Babesia symptoms but tested positive on the FISH, do I need to go through the treatment. I am mid 60 and very thin. Multiple Chemical sensitivities from exposures,. MAST cell activation,. Chronic Inflammatory Response, etc….. What are your thoughts? Oh Babesia did also appear via a homeopathic type of test earlier this year but I failed to complete his natural therapy. Do you recommend additional testing or is the IGEnIX FISH the Gold Standard? Would you perform other tests? Oh, with the Mycotoxins still present I hate to bring more opportunities for mold in me. My GI system is also under duress. Other organs stressed, too.
I have Lyme disease patients who have a wide range of positive tests. It is difficult to determine what direction to take. I have patients who have improved with Babesia treatment even without a positive test.
The treatments helped. This ìs an epidemic with how the number of disease cases have skyrocketed.
Hello. I had a tick removed 2 weeks ago that was embedded in my back for 5 days. The tick was sent off for independant testing and came back positive for babesia odocoilei. I started a protocol of herbs (crypto, bidens pilosa, sida) and have spoken with several ND’s and LLND’s here in Ontario, Canada with one suggesting ivermectin and another suggesting the antiobiotic combo of zithro and mephrone. I prefer not to do the antiobiotics and want to try the ivermetin. Do you have any experience or suggestions in dosing?
hi Sue, curious which lab you used that tested for odocoilei? This is not very common and I’d love to know! Since your infection was brand new and you didn’t report being sick I believe doxycycline for 8 weeks was likely all you needed, but what did you end up doing?
Dr. Cameron, I did low dose disulfiram on and off for several months over the past year. Each time i have ended up with dizziness, nausea, headaches, and revelry with heart palpitations and extreme fatigue. My reaction to DSF is making me suspect that treatment with it might be stirring up Babesiosis. I’ve never had a positive test but have had Lyme for many years and also got a new tick bite about a year ago. I had the tick tested and it tested negative for Babesiosis. However, I have been declining in health even from my previous status for several months. Would taking Mepron or Malarone give me a treatment reaction that might indicate the presence of an infection with Babesia? Also, I am in peri menopause, so struggling to distinguish between those symptoms and unresolved tick borne illnesses.
I have patients in my practice who need to find Malarone/Mepron helps.
Diagnosed 3 weeks ago with Lyme, Babiosa and Covid 19 .
Now have AFIB , hopefully will go away soon
What a stretch for recovery.
I assume you are also working with a cardiologist. Get well soon.
Dr Cameron, if a Hematologist says he seen Babesia on a smear, is a positive PCR needed for confirmation? My Hematologist says he saw Babesia on 2 out of 3 smears, but will not treat because confirmatory PCR through Mayo was negative.
The Babesia parasite clears without treatment. I have had some patients whose PCR and antibodies are negative yet do well with treatment for Babesia.
Hi Dr Cameron. First, thank you for the wonderful work you are doing. Your office has already been very helpful to me and I couldn’t be more grateful. I was bitten by at least 2 ticks in Slovenia in October. Based on the evidence I have (which isn’t perfect of course), it looks like one of the ticks was a sheep tick and had been attached for 1-2 days. I started doxy (100 mg, 2x a day) at apx the 48-hours-after mark. Then, after returning home, I saw a lyme specialist on the US west coast who recommended doubling that (200 mg, 2x a day) while waiting until enough time had passed to do more testing. She tested me for lyme and babesia using igenex. The lyme test shows 3 bands positive (weak, 1 +) and shows the strain as a U.S. strain. All the Babesia tests who negative except for the FISH test, which shows positive. She is suggesting 6 months of Malarone (as well as testing for additional infections). I have had no symptoms at all, except for 3-4 days after returning home from Slovenia, at which time I felt very tired and sort of mentally slow, but that could have been jet lag (though it was worse than any jet leg I’d ever experienced). If I didn’t know anything of this was happening, I wouldn’t think anything was going on with me physically. I run 5-6 miles 3 times a week, lift weights, as I have been doing for years and am not noticing anything unusual.
Having read that Babesia usually clears up on it’s own, I was already skeptical about taking 6 months of Malarone and then my pharmacy told me that the manufacturer of Malorone says it is out of stock. If you were me, would you do anything about the positive FISH babesia? And/or what would you recommend for a patient? If there is a likeliness that it will clear up on it’s own, I prefer to let that happen. I would want to avoid a situation where it flares up down the road too though. I was diagnosed with hashimotos 20 years ago, other than that, no health issues.
Do you do second opinion appointments virtually?
Again, thank you SO MUCH for what you are doing.
Just turned 55, and can trace the first Lyme, maybe more, infection back to three months before I turned 9. Well before it had the name we now know it by. Most likely, I was infected at birth, given the issues I had. It was all tossed under Woodsman’s Disease back then and you were taught not to let others know, never show pain or anything else.
In the last four years I have been diagnosed with Lyme, Neuro Lyme, Babesia, Bartonella, CMV, Anaplasmosis, Hashimoto’s, severe diabetes symptoms, but those are a red herring, MCAS, CIRS/SIRS. Could not afford a full panel through IgeneX, so, the thought is there is more.
Double bypass 4 years 4 months ago. After a year of complaining to deaf ears, convinced a cardiologist to do a stress echo, then he did another heart cath. His words when done, “F&**, you were right, their surgery didn’t work. The whole bottom part is closed. Nothing we can do, no stent, no surgeries, just hope to find a working med. You will be lucky to get 2 years.” Well, I am still alive, but have no quality of life. I haven’t been able to read a book i over 10 years. Just this little comment, wipes me out. My DO told me yesterday tha the hoped I had a signed DNR order on file everywhere and on my person. Gee thanks for the vote of confidence doc. I have 3 to 5 nitro patches on 24/7 and take up to 10 nitro tablets a day. And my BP will still shoot up to 231/140 hr 115….or similar. My average is 197/101 pulse preferably under 72 or I end up with heart attacks (spill troponin and all), chest pain, down the arms, into jaw and the brain. Fun times.
I am wondering now if some of this isn’t Babesia related instead of Lyme?????
Good thing I am stubborn. Oh, and disability is denied because my EKG barely shows a blip.
In your opinion which is more effective for treating Babesia; Mepron or Malerone?
I just want anyone who will listen to know that my husband had a psychotic episode just before he was taken to a hospital and diagnosed with Babesiosis. He went on a shopping spree emptying our bank accounts (he NEVER shops) and then proceeded to destroy our downstairs. He thought he was “cleaning” but he was destroying everything in his path. 6 days later, he remains in the hospital and still thinks all he was doing was normal. I have read case studies and this is an extremely dangerous disease that includes psychosis and I think more attention needs to be paid to that and hospital personnel need more education, especially that fact that this is NOT Lyme.
I pray your husband recovers soon.
Hi I was bit on 8/13 by a tick in Pennsylvania, few days after got knee pain and my igm came back abnormal . was put on doxycycline after 2 days I developed tremors in my hands , they put me on another med and the tremors continued but eased up, I was told to stop them and now I still have fatigue, tremor in my hands and body , I can’t repeat labs until 9/15 to get a real read they claim so here I sit and wait . I see a Funtional med lady and she tested me high for babesios but my primary said that cant be determined unless under microscope . I have anxiety and ptsd as it is and this tremor stuff is scary and the not knowing . Is tremors common ?
Tremors alone are seen in a wide range of conditions. Some doctors are reluctant to recognize Babesia unless the parasite is seen in the red blood cells. I don’t agree. I have patients who don’t become positive for Lyme after even a few days of antibiotics. I have had to use clinical judgment. I have patients who I have had to refer to specialists to rule out other illnesses at the same time.
I had a14 percent parasite level when diagnosed. Treated for 10 days with azithromyicin Avitoquoine. 2 months later still feel sick ID doctor had me do 7 more days. But blood tests show DNA. 3 months more and i still feel awful. Any advice?
I was bitten by something in dec 2024 and 3 days later had tremor episode with month long flu like symptoms. fever 100
i had facial droop randomly, eyes issue (teary,floaters),loss of appetite, burning pain in arms and legs, heaviness in head and scalp pain,numbess tingling in legs and arms,shoulder joint pain,neck stiffness.
neurologist did EMG eeg and said i have lumbar radiculopathy ,cervical radiculopathy
MRI brain scan had some scattered white matter which they said its common from chronic migraines
i never had headaches before this bite episode
first 1 month i had severe anxiety, heart palpitations, high blood pressure, uncontrolled emotional behavior
things subsided now except headache and fatigue.( i did IV vitamin infusions, ton of supplements etc )
After many visits to doctor and all an LLMD tested me .i have only Babesia positive in igenex test.I will ne meeting him in 10 days.
question is should i treat it now or let my body take care of it.
next can i not have lyme but just babesia(i am in south florida)
how long should i treat to make sure its gone .( as its parasites)
can you use herbs while taking antibiotics.
Doctors differ in their approach. I am not in favor of sitting on a potential tick borne infection or taking an herbal approach first.
I took just 1 week of doxycyclin after my bite ( 3 weeks after) i had no rash.
could that be the reason my igenx lab shows negative on lyme but it shows babesia on FISH test
doxycycline doses not work for Babesia