Neonatal babesiosis is a rare but serious threat to premature infants. A team of researchers at Yale School of Medicine describe three premature infants—all in one neonatal intensive care unit—who contracted Babesia from a single 24-year-old blood donor.
The report was published in the Pediatric Infectious Diseases Journal.
How Neonatal Babesiosis Spread Through One NICU
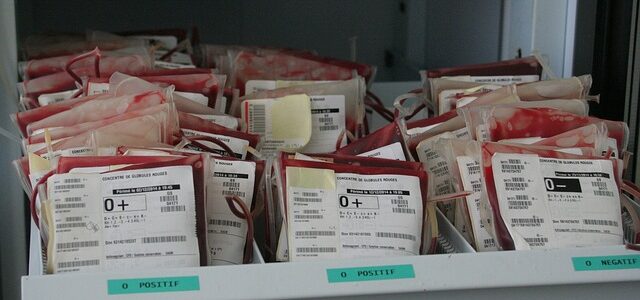
Babesia is a particularly frightening infection, given that it can be unknowingly transmitted to multiple people through blood banks, which have no foolproof way of screening donors.
“Screening questionnaires are clearly insufficient given the growing number of cases of transfusion-transmitted babesiosis,” writes Glanternik from the Division of Infectious Diseases, Department of Pediatrics at Yale School of Medicine.
The 24-year-old donor from Connecticut was not flagged by the blood bank and “was deemed suitable for donation by the American Red Cross and his serology was negative for all FDA-mandated tests,” Glanternik explains.
This case echoes broader concerns about Babesia in the blood supply.
Neonatal Babesiosis: Three Infants Infected
Three premature infants contracted Babesia from this donor, with two developing high-grade parasitemia (presence of parasites in the blood), according to Glanternik:
- Infant A: Parasitemia peaked at 13.4%
- Infant B: Parasitemia peaked at 12.5%
- Infant C: Parasitemia peaked at 6.8%
These are dangerously high levels. For comparison, parasitemia above 10% often requires exchange transfusion in adults.
Treatment of Neonatal Babesiosis
All three premature infants were treated with a combination of azithromycin and atovaquone despite published recommendations for clindamycin and quinine.
“The stability of oral suspension [of quinine] using capsules is undetermined,” explains Glanternik. “Furthermore, quinine’s narrow therapeutic index and potential adverse effects limits its utility in treating small children.”
The infants were treated for 14 days—longer than the 7-10 day recommendation described in the IDSA guidelines.
Relapse After Treatment
However, more than a month (48 days) after treatment, one of the infants relapsed. There were no specific signs that could be attributed solely to babesiosis, explains Glanternik. But a “routine blood smear demonstrated relapse with 1% parasitemia.”
By day 9 of retreatment, the smear was negative. Treatment continued for a total of 23 days. None of the three premature infants required exchange transfusions.
This relapse pattern is consistent with other cases of persistent Babesia that require extended treatment.
Detecting Neonatal Babesiosis Is Difficult
“Clinicians should maintain a high index of suspicion for neonatal babesiosis in an infant who has received a transfusion because the clinical manifestations and concomitant lab abnormalities are non-specific and resemble those present in prematurity even in the absence of infection.”
This is similar to challenges faced when diagnosing Babesia in other infants—symptoms overlap with many other conditions.
Questions This Case Raises
- Would longer initial treatment have prevented a relapse for Infant C?
- What are the consequences for infants if Babesia is not detected by thick smear?
- How can doctors be sure their newborns are clear of Babesia after the blood smear turns negative?
Editor’s Note
This case demonstrates why current blood bank screening is inadequate. A healthy 24-year-old donor passed all FDA-mandated tests yet infected three vulnerable premature infants.
The relapse in Infant C—48 days after completing treatment—shows that even 14 days of therapy may not be enough for neonatal babesiosis. Standard IDSA guidelines recommending 7-10 days would have been even less adequate.
We need universal Babesia screening for blood donors, especially in endemic areas like Connecticut and New York.
Frequently Asked Questions
What is neonatal babesiosis?
Neonatal babesiosis is a Babesia infection in newborns. It can occur through transfusion of infected blood or transmission from mother to baby during pregnancy.
How did three infants get infected from one donor?
Blood from a single 24-year-old donor was used for multiple transfusions in a neonatal intensive care unit. The donor passed all standard screening tests but was infected with Babesia.
Why did one infant relapse?
Infant C relapsed 48 days after completing 14 days of treatment. This suggests that even extended treatment may not fully clear the infection in some cases.
How is neonatal babesiosis treated?
These infants received azithromycin and atovaquone for 14 days. Quinine-based regimens are typically avoided in infants due to safety concerns and dosing difficulties.
Can blood screening prevent neonatal babesiosis?
Current screening questionnaires are insufficient. The donor in this case passed all FDA-mandated tests. More comprehensive Babesia-specific screening is needed.
References
- Glanternik JR, Baine IL, Tormey CA, Rychalsky MR, Baltimore RS. A Cluster of Cases of Babesia Microti Among Neonates Traced to a Single Unit of Donor Blood. Pediatr Infect Dis J. 2017.
- Wormser GP, Dattwyler RJ, Shapiro ED, et al. The clinical assessment, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006;43(9):1089-1134.