Call for your appointment today 914-666-4665 | Mt. Kisco, New York
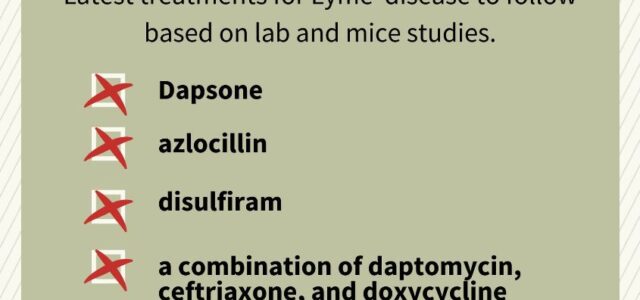
Study findings suggest that current Lyme disease treatment may not eliminate the Borrelia burgdorferi infection or the immune system may fail to clear the infection or bacterial debris, resulting in ongoing symptoms. In the past few years, several new treatments for Lyme disease have been investigated in the laboratory or made available to patients in an effort to address chronic symptoms.
Although still in the early stages, two new treatments for Lyme disease seem to show promising results. Published case reports describe the effectiveness of dapsone, an antibiotic typically used to treat skin conditions and disulfiram, frequently prescribed for alcohol abuse.
Dapsone
Horowitz et al. reviewed data from 200 patients to evaluate “the efficacy of dapsone combined with other antibiotics and agents that disrupt biofilms for the treatment of chronic Lyme disease/post-treatment Lyme disease syndrome (PTLDS).” [2]
They found that it “decreased eight major Lyme symptoms severity and improved treatment outcomes among patients with chronic Lyme disease/PTLDS and associated co-infections.”
This new treatment for Lyme disease was not without side effects, however. Horowitz reports 46 of the 200 patients stopped treatment due to an “adverse reaction.” The adverse effects were not specified.
When used for other conditions, dapsone’s side effects have included haemolysis, agranulocytosis, photosensitivity, skin eruptions, neuropathy, and toxic or cholestatic hepatitis. [3]
Disulfiram
Disulfiram, a medication used to treat alcohol abuse, may be one of the new treatments for Lyme disease in the near future. Two small studies have shown positive results.
Dr. Kenneth Liegner reports that 3 patients, who required extensive, ongoing antibiotic treatment due to neurological Lyme disease and Babesia, “were able to discontinue treatment and remain clinically well for periods of observation of 6–23 months following the completion of a finite course of treatment solely with disulfiram.” [4]
One patient did relapse at 6 months and was re-treated with disulfiram.
READ MORE: 6 reasons for delayed treatment of Lyme disease
The results from another group of 30 patients who received disulfiram were described by Liegner during the 2019 International Lyme and Associated Diseases Society (ILADS) annual conference. “Results have been impressive, and disulfiram use, with careful supervision, has been relatively safe.”
“It will remain to be seen whether disulfiram has a role in acute or early Lyme disease or babesiosis,” Liegner adds.
Furthermore, “Any role for disulfiram in children, with their incompletely matured nervous systems, remains to be determined and should be approached with caution, as there is little experience with its use in children.”
None of Liegner’s three patients stopped treatment with disulfiram. One patient had a temporary psychiatric hospitalization, and a second stopped after a syncope event that led to a concussion that required hospitalization. And according to Liegner, the risk of adverse events was even lower in the study involving 30 patients.
Disulfiram’s side effects, when prescribed for other conditions, have included “encephalopathy, convulsion, cranial and peripheral neuropathy, toxic optic neuropathy, irreversible injury to the basal ganglia with permanent neurological deficits, hypertension, and drug-induced psychosis, presumably due to the inhibition of dopamine beta-hydroxylase,” writes Liegner.
Another study investigating disulfiram as one of the new treatments for Lyme disease and co-infections was launched in 2019 by Dr. Brian Fallon, from the Lyme and Tick-Borne Diseases Research Center at Columbia University.
Azlocillin
A study by Stanford Medicine suggests that the antibiotic azlocillin “completely kills off the disease-causing bacteria Borrelia burgdorferi at the onset of the illness.” In addition, the authors say, azlocillin “could be effective for treating [Lyme disease] patients infected with drug-tolerant bacteria that may cause lingering symptoms.” [5]
Researchers tested azlocillin in mice infected with Lyme disease at 7-day, 14-day and 21-day intervals and found that it eliminated the infection. Additionally, in lab dishes, the azlocillin killed drug-tolerant forms of B. burgdorferi, “indicating that it may work as a therapy for lingering symptoms of Lyme disease,” according to the Stanford team.
Azlocillin has not yet been prescribed or studied in Lyme disease patients.
[bctt tweet=”Promising new treatments for chronic Lyme disease symptoms could be on the horizon. ” username=”DrDanielCameron”]
Azlocillin adverse events for other indications have included hypersensitivity reactions, hypocalaemia, hepatotoxicity, diarrhea, and leukopenia. [6] There are also costs and risks associated with the need to administer azlocillin intravenously.
Combination: daptomycin, doxycycline, and ceftriaxone
Researchers from Johns Hopkins School of Public Health found that a combination of antibiotics – daptomycin, doxycycline, and ceftriaxone − eradicated the slow-growing variant form (persisters) of the Lyme bacteria in a mouse model. Scientists believe persisters may be responsible for the chronic symptoms that some Lyme disease patients experience.
“There is a lot of excitement in the field because we now have not only a plausible explanation but also a potential solution for patients who suffer from persistent Lyme disease symptoms despite standard single-antibiotic treatment,” says Ying Zhang, MD, Ph.D., senior author on the study. [7]
Zhang and his team hope to test the drug combination in people with persistent Lyme disease.
Daptomycin has not yet been prescribed to Lyme disease patients, and adverse effects, for other conditions, have included myopathy/rhabdomyolysis, eosinophilic pneumonia, and anaphylactic hypersensitivity reactions. [8]
There are also costs and risks associated with the need to administer daptomycin intravenously.
Editor’s note: I am encouraged by all the research seeking to identify new treatments for Lyme disease and remain hopeful that we will develop research designs to evaluate the value of these and other treatments for tick-borne diseases.
Related Articles:
Will late-stage Lyme disease treatment include azlocillin?
Is prolonged treatment for Lyme disease the new norm?
Persister cells survive attacks by antibiotics and may contribute to chronic illness in Lyme disease patients
References:
- Adrion ER, Aucott J, Lemke KW, Weiner JP (2015) Health Care Costs, Utilization and Patterns of Care following Lyme Disease. PLOS ONE 10(2): e0116767. https://doi.org/10.1371/journal.pone.0116767
- Horowitz RI, Freeman PR. Precision medicine: retrospective chart review and data analysis of 200 patients on dapsone combination therapy for chronic Lyme disease/post-treatment Lyme disease syndrome: part 1. Int J Gen Med. 2019;12:101-119.
- Wozel G, Blasum C. Dapsone in dermatology and beyond. Arch Dermatol Res. 2014;306(2):103-124.
- Liegner KB. Disulfiram (Tetraethylthiuram Disulfide) in the Treatment of Lyme Disease and Babesiosis: Report of Experience in Three Cases. Antibiotics (Basel). 2019;8(2).
- Pothineni VR, Potula HSK, Ambati A, et al. Azlocillin can be the potential drug candidate against drug-tolerant Borrelia burgdorferi sensu stricto JLB31. Sci Rep. 2020;10(1):3798.
- Parry MF. The tolerance and safety of azlocillin. J Antimicrob Chemother. 1983;11 Suppl B:223-228.
- Feng J, Li T, Yee R, et al. Stationary phase persister/biofilm microcolony of Borrelia burgdorferi causes more severe disease in a mouse model of Lyme arthritis: implications for understanding persistence, Post-treatment Lyme Disease Syndrome (PTLDS), and treatment failure. Discov Med. 2019;27(148):125-138.
- Patel S, Saw S. Daptomycin. In: StatPearls. Treasure Island (FL)2020.




Hello Doctor: Thanks for the great work you are doing for Lyme patients. As a 72 year old male with late-stage neuro Lyme who’s been treated for 12 years, I feel that azlocillin may be my only hope. When do you expect that it may be available as an oral medication? FYI, I tried disulfiram at full-dose for 3 mos. 6 days but had to stop due to severe psych symptoms. I did receive some benefit from it.
I am not sure when azlocillin will be available. It is a shame the disulfiram did not work for you.
From what I’ve read about azlocillin, it doesn’t cross the blood-brain barrier very well if at all, so it might not be very useful.
Does the Pill version of Azlocillin safe to take.
I have had 4 acute Lyme infections – 3 had bites associated. The most recent did not, but I tested positive 2/3 months after my prior acute infectionn – for which I took antibiotics for a few weeks.
I’m baffled why I keep getting bit
And NOW – the antibiotics don’t seem to help much. The symptoms go away for a week or so and then come back with a vengence.
I purchased from GoldBio.com pill version of azlocillin. Is it ok to take
The azlocillin is not yet available. I would have to look at the side effects if it become available. I do not have any experience with GolBio.
I can only find dr Horowitz protocol online from 2020. Is there a newer version available?
Yes, he goes over the new protocol in the LivLymeFoundation conference lecture he gave last year. You can get it on the LivLymeFoundation for free by going to their site.
I have lyme, babesiosis, anaplasmosis, bartonella for over 7 years. I’ve paid tons of money on medical treatments that insurance does not cover. I’m at my witts end and could argue, it’s not these that will cause my death…it’s the not knowing. My question is…what is the parasite living in my skin. NO, I DO NOT have delusions of parasitosis, ive never had it and truly want to curl up in a ditch while someone covers me with dirt if one more doctor tells me that. I’m not illiterate, I’m not a hypercondriac, I’m not mentally ill..YET. I am losing my balance, my feet have what feels like ants crawling, burning, numb, utterly unable to sleep, walk or work because of it. What I really need to know is what skin parasite is in my skin, I see them, they are microscopic…they can be seen by microscope at 100x. I only wanted to see this not the things we all have living on us…those things don’t bite, only these things that have now completely taken over my skin. I don’t know how to describe this, I don’t have a microscope, but a friend had an old one and I couldn’t hook up a camera to it. It’s so frustrating when I can’t get help for a skin parasite, and instead told I’m nuts. Any information that may help me would so much appreciated I cannot give a big enough thank you or God bless you. Just know that I will hold you in my heart, forever. I don’t want to die with these things in my body. One of these diseases is causing heart failure, spots on my liver and spleen, and kidney problems, to name a few of my organs that are being damaged, and my skin in a total take over…this being my largest organ, I simply want to know what these parasites may be, and how to fight them. Thank you so much for taking the time to read this, you’ve already done more than my drs.
I have had Lyme patients who present with lesions described by Morgellons patients. They have not found parasites. I have often found treatment helpful if I treat their underlying Lyme disease.
Hi melony
I have been sick for 15+ years.i was misdiagnosed with Lupus. My heart, ,skin, liver, eyes, muscles, brain, basically everything was slowly becoming destroyed. I started a year ago spending over $50,000+ on blood work, meds, etc…on a mission to find my illness. I never believed it was lupus. I had crazy skin conditions that could range anywhere from head to toe. I bought a microscope as part of my mission. I have always had bouts of thinning hair, but out of nowhere it started feeling like glass in my scalp. I had taken a piece of tape and stuck it on the back of my head. Under the microscope I could see what looked like balls of hair all tangled. I used google lens to search for similar images. The results kept coming back with photos that looked identical, but said they were Morgellan’s disease. I had started my first month of treatment for Lyme disease prior to seeing this. I literally lost my mind because the last thing I wanted to think I had was Morgellan’s. If you do any research on this topic, you will find it is highly controversial, although I did find a lot that do say It does appear in people who have had Lyme. There is something that I did see under the microscope from my scalp which is absolutely an image of parasite. I know exactly how to identify the Demodex mites, scabies, lice, because I actually thought I must’ve had some type of parasite in my skin all these years. This is absolutely different and when I match it with Google lens, it comes up with some similar looking thing, but it definitely is not. I don’t know if this is Morgellan’s but I have seen images that have been posted of something similar on Morgellan’s sites. I do not even say that word to anyone, except Dr Cameron. Last thing I want is all of my 20 doctors over the years who are furious that I went and found what was really wrong with me now saying I am going nuts. I have slides and photos if you would like to see them. Just let me know.
Girl you absolutely have morgellons disease. Get the book on Amazon by Ginger Savely. I also have it and was unaware of my own Lyme disease but the crawling and fibers/ hairs is a tell tale sign. It feels like parasites and I was also convinced but it is bacterial. I’m still being treated and we will see but I know I am not crazy and it is very isolating. Hang in there
(I am 21 having seizures out of nowhere because of Lyme) Hello, 3 years ago my left knee swelled up. I was immediately tested and diagnosed with Lyme. After 6 months of extensive pills and a month of daily IV and hyperbaric treatment I left those doctors and found one that would give me a DMARD (disease modifying Anti Rheumatoid Drug) my knee swelling went away within 2 weeks. I was still dealing with immense brain fog, extreme anxiety, and occasional panic attacks. Then I started getting focal seizures (auras) that consisted of extreme Deja vu, I start to hear the world in a strange way. Someone could be talking to me and I am unable to understand them/contemplate what they are saying, yet I feel as if I am able to predict the next words to come out of their mouth. Almost like I hear a voice in my head. The sensation lasts for 45 ish seconds and once it’s done I have little to no memory of what I had said or was thinking. I have recorded myself saying what’s in my head when I can get to my phone and what I find is myself speaking literal gibberish. Then a year ago I had a grand mal in my sleep (I was sleeping with my girlfriend) I’ve had about 5 in the past year all in my sleep and I have multiple focal seizures every day. No one knows what to do with me. Neurology just want to put me on epileptic medication but I’m scared to do that. See I believe I made a mistake in taking the DMARD. I fixed the symptom but not the underlying Lyme. And without that visual problem I just went on with my life and in doing so let the Lyme worsen to the point of seizures. I fear taking the epilepsy medication is essentially doing the same thing, a bandaid on a bullet hole. And if i take the meds without a plan to combat the underlying Lyme, the seizures may go away and I move on with the potential of worsening the Lyme. I see the possibility of dementia when I research this and I am very much not willing to get that. If anyone has any advice I would very much appreciate it.
Dr Daniel Cameron
I would like you to email me at al*********@****oo.com
I am a long term late stage lyme client / survivor as now quiet a nutritionist. I would like to have you contact me.
Connie Allie Jenkins’
My husband got a false negative from John’s Hopkins Dec 2023 and had myocarditis and was hospitalized for 3 days which the doctors didn’t know what was wrong with him and cost us after insurance $9k and had inflammation, chronic fatigue and got an autoimmune Hashimotos and brain fog and almost fainted a few times because of this false negative or misdiagnoses and has been suffering for years with lyme disease!!! Until he went to a holistic NAET center called Elevate Life in Annapolis, MD and Dr Johns and got the correct blood test, were they able to find the lyme disease and only IV laser treaments and lecher antennae treatments so far are helping him and for many they claim they are lyme free from doing the laser treatments ..why don’t they avocate this for lyme month??? Antibiotics don’t help since it doesn’t get through the hard biofilm that the lyme bacterium hide and stay dormant and so lyme attacks again after weeks of antibiotics or herbs and is so difficult to treat and so people with lyme suffer for years with autoimmune and fatigue and seizures and inflammation etc and therefore the only cure is IV laser treatments (Lyme Laser Centers) which the laser can get through the biofilm but it’s not covered by most insurance and can cost $10k+ when a lot of people are still getting a false negative but no doctors are discussing this with their patients!!!