New study by guidelines author dismisses risk of chronic Lyme disease
There is a growing body of evidence demonstrating the existence of chronic manifestations of Lyme disease. These studies have found that the Borrelia burgdorferi (Bb) infection can cause chronic illness, even when the standard 14- to 21-day antibiotic treatment regime is initiated in the early stages of the disease. [1,2] Additional research has also found that these patients have a high risk of an impaired quality of life. [3,4]
by Daniel Cameron, MD, MPH
Physicians use various terms when referring to chronic manifestations of Lyme disease ─ Lyme encephalopathy, Chronic Lyme disease (CLD), Post-Lyme disease syndrome (PLDS), or Post-treatment Lyme disease (PTLD).
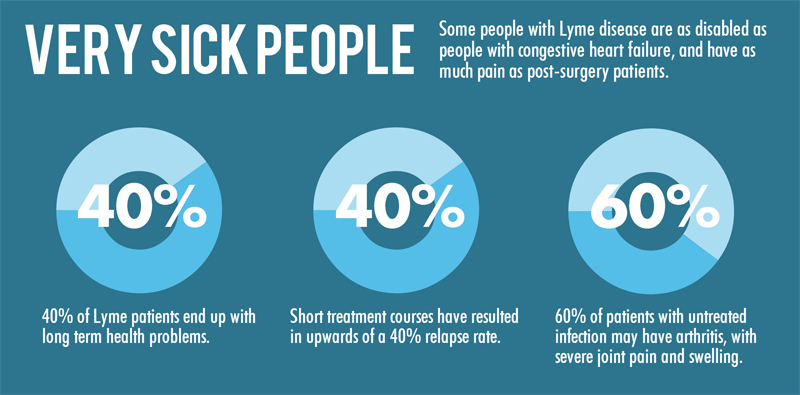
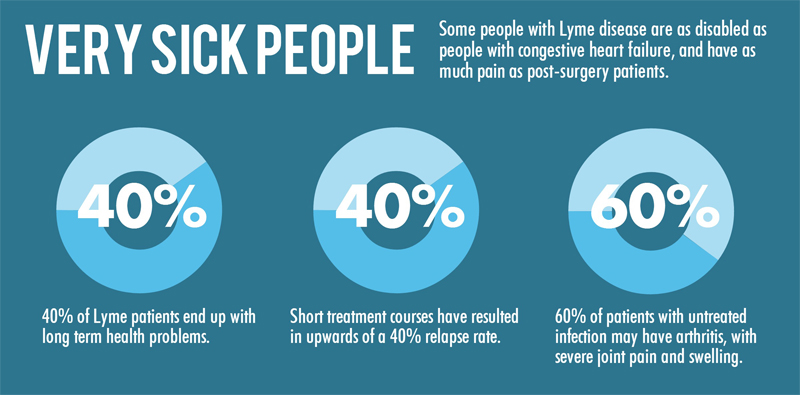
The National Institute of Health (NIH) conducted four separate trials, which validated the existence, severity [5,6] and duration [5,6] of chronic manifestations of Lyme disease. A 2001 study by Klempner and colleagues found, “the deficits in physical health status … were equivalent to those observed in patients with congestive heart failure or osteoarthritis.” [4]
Another study by Dr. Brian Fallon, published in Neurology found, “reports of pain were similar to those of post-surgery patients, fatigue was similar to that of patients with multiple sclerosis (MS), and limitations in physical functioning were comparable with those of patients with congestive heart failure.” [3]
In a study published in this month’s Clinical Infectious Diseases, Dr. Gary Wormser and colleagues access the existence of chronic manifestations of Lyme disease and the impact it has on a patient’s long-term quality of life. [7]
The study examines the health related quality of life for 283 culture-confirmed Lyme disease patients, who presented with erythema migrans (EM) rashes. [7] The patients were evaluated 11 to 20 years after treatment, which involved the standard antibiotic regime.
Patients were on average 65 years old with 81% having an EM rash and 19% having multiple skin lesions at their initial visit. Of the 283 patients, 100 remained enrolled in the study, which found that 11 to 20 years after treatment, the quality of life for these patients was “virtually identical” to the general population.
In addition, these patients were not more prone to developing fibromyalgia and/or chronic fatigue, according to two additional papers by Dr. Wormser. [8,9] The second paper found only 1 out of the 100 patients (1%) developed fibromyalgia and that patient developed it 19 years after the Lyme disease diagnosis – suggesting no correlation. [9] The third paper reported that only 9 patients (9%) complained of severe fatigue.[8]
“This study should help suppress concerns that the effects of early Lyme disease
are likely to cause lifelong debilitation.” – Dr. Paul Auwaerter
In essence, all three paper suggested that if a Lyme disease patient is treated at the early stage of the disease, with the standard antibiotic protocol, they will not develop any long-term symptoms that would negatively impact the quality of their life.
At first glance, the study results support the message that Lyme disease does not cause chronic illness and a diminished quality of life. However, upon further inspection, the reader might find the message to be somewhat misleading.
Such findings by Wormser and colleagues would be expected, given the patients were treated an average of four days after the onset of illness. Identifying, diagnosing and initiating treatment for Lyme disease within days of symptom presentation is unusual. In fact, treatment delays average two years, according to several studies. [3,10]
Additionally, the study did not include patients who had extracutaneous manifestations of Lyme disease, which would include those with chronic neurologic Lyme [11] and Lyme encephalopathy. [12]
In contrast, there are studies which have shown chronic manifestations of Lyme disease do exist, [1-4] can be severe, [3,4] last for years [3,4] and be life altering for patients. These studies include patients with extracutaneous manifestations, as well as those who began treatment after the four days of illness onset. [1-4] These studies confirm the existence of chronic Lyme disease and the detrimental impact it can have on a patient’s life.
A retrospective cohort study in Massachusetts found 34% of patients had arthritis or recurrent arthralgias, neurocognitive impairment, and neuropathy or myelopathy, an average of 6 years after treatment for Lyme disease.
Another study in Westchester County, New York, examined a cohort of 215 consecutively treated Lyme disease patients and reported that 62% suffered from arthralgias, arthritis, and cardiac or neurologic involvement with or without fatigue a mean of 3.2 years after treatment. [1]
And previous studies report there’s a high risk of developing fibromyalgia after having Lyme disease. Nearly half (49%) of 788 patients evaluated in a Lyme disease center were diagnosed with fibromyalgia shortly after objective manifestations of Lyme disease. [13]
Unfortunately, when reviewing the Wormser study at a glance, most physicians would conclude that Lyme disease does not cause chronic manifestations nor does it lead to a diminished quality of life for patients. And, in turn, those physicians cite the study with colleagues and in other published papers and perpetuate a message that on the surface is positive. But, upon closer inspection, is misleading.
For instance, Dr. Paul Auwaerter, of Johns Hopkins University School of Medicine, gives substantial attention to the study in an article he wrote entitled, “Life after Lyme disease,” published in this month’s issue of Clinical Infectious Diseases. [14] “Wormser and colleagues have contributed valuable information that should help allay the common distress that Lyme disease is routinely life-altering for the long-term.” [14] In the same paper, he states “this study should help suppress concerns that the effects of early Lyme disease are likely to cause lifelong debilitation.” [14]
Meanwhile, Dr. Paul Lantos, from Duke University School of Medicine, repeats the message in another published paper, stating “only 1 of 100 patients treated for culture-confirmed Lyme disease developed fibromyalgia during the subsequent 11 to 20 years.” [15]
And so the message is cited over and over, read by thousands of medical professionals who take the study results at face value, and not necessarily examine the intricate details or design of the study population.
In fact, the study design is praised by Dr. Auwaerter. “They have followed an extremely well-characterized cohort of patients with treated early Lyme disease … who had their infection unquestionably confirmed. … “
He continues, “These patients fared no worse and even better than average in all eight measured sphere, suggesting that Lyme disease did not have an ongoing impact on their health at the time.”
Dr. Wormser’s findings cannot be generalized to actual practice because of the severe limitations of the study. In actual practice there are patients who are sicker longer than 4 days before treatment is begun and who present with extracutaneous manifestations of the disease, such as neurologic Lyme and Lyme encephalopathy.
A sizeable group of patients was excluded from the study. In the interest of patients, this group needs to be recognized and included in such studies if there is to be any real progress in understanding the true impact of this disease – physically, socially and financially – on patients.
References
1. Asch ES, Bujak DI, Weiss M, Peterson MG, Weinstein A. Lyme disease: an infectious and postinfectious syndrome. J Rheumatol, 21(3), 454-461 (1994).
2. Shadick NA, Phillips CB, Logigian EL et al. The long-term clinical outcomes of Lyme disease. A population-based retrospective cohort study. Ann Intern Med, 121(8), 560-567 (1994).
3. Fallon BA, Keilp JG, Corbera KM et al. A randomized, placebo-controlled trial of repeated IV antibiotic therapy for Lyme encephalopathy. Neurology, 70(13), 992-1003 (2008).
4. Klempner MS, Hu LT, Evans J et al. Two controlled trials of antibiotic treatment in patients with persistent symptoms and a history of Lyme disease. N Engl J Med, 345(2), 85-92 (2001).
5. Klempner MS. Controlled trials of antibiotic treatment in patients with post-treatment chronic Lyme disease. Vector Borne Zoonotic Dis, 2(4), 255-263 (2002).
6. Tager FA, Fallon BA, Keilp J, Rissenberg M, Jones CR, Liebowitz MR. A controlled study of cognitive deficits in children with chronic Lyme disease. J Neuropsychiatry Clin Neurosci, 13(4), 500-507 (2001).
7. Wormser GP, Weitzner E, McKenna D et al. Long-term Assessment of Health-Related Quality of Life in Patients With Culture-Confirmed Early Lyme Disease. Clin Infect Dis, (2015).
8. Wormser GP, Weitzner E, McKenna D et al. Long-Term Assessment of Fibromyalgia in Patients with Culture-Confirmed Lyme Disease. Arthritis & rheumatology, (2014).
9. Wormser GP, Weitzner E, McKenna D, Nadelman RB, Scavarda C, Nowakowski J. Long-term assessment of fatigue in patients with culture-confirmed Lyme disease. Am J Med, 128(2), 181-184 (2015).
10. Cameron DJ. Consequences of treatment delay in Lyme disease. J Eval Clin Pract, 13(3), 470-472 (2007).
11. Logigian EL, Kaplan RF, Steere AC. Chronic neurologic manifestations of Lyme disease. N Engl J Med, 323(21), 1438-1444 (1990).
12. Logigian EL, Kaplan RF, Steere AC. Successful treatment of Lyme encephalopathy with intravenous ceftriaxone. J Infect Dis, 180(2), 377-383 (1999).
13. Steere AC, Taylor E, McHugh GL, Logigian EL. The overdiagnosis of Lyme disease. Jama, 269(14), 1812-1816 (1993).
14. Auwaerter PG. Life After Lyme Disease. Clin Infect Dis, (2015).
15. Lantos PM. Chronic Lyme Disease. Infect Dis Clin North Am, 29(2), 325-340 (2015).




Barbara Ann Briguglio
03/19/2019 (12:27 pm)
It looks like extremely “restrictive “ study by Wormser et al was so severely one sided, but also very selective on subjects. Extremely misleading and allowing me to believe that it was purposely funded to create this so called end result finding. It seems he and his cohorts are still being paid to make the end results fit the study, ergo false and incorrect information being fed to the scientific community that know Chronic Lyme is real. It makes him look like he is being intentionally paid to create falsehoods towards the subject at hand.
NEW STUDY BY GUIDELINES AUTHOR DISMISSES RISK OF CHRONIC LYME DISEASE by Daniel Cameron MD | To Lyme and Back
06/26/2015 (12:38 am)
[…] https://danielcameronmd.com/new-study-by-guidelines-author-dismisses-risk-of-chronic-lyme-disease/ […]
Phyllis Mervine
09/08/2015 (2:15 am)
As you say, this is a big problem: “in turn, those physicians cite the study with colleagues and in other published papers and perpetuate a message that on the surface is positive. But, upon closer inspection, is misleading.”
I call this the “disinformation echo chamber.” People who do not read the research too carefully, uncritically accept the conclusions of the study authors, including their misrepresentations of previous studies.. Hence the original misinformation becomes amplified and exaggerated over time, as in the children’s game, Telephone. Thank you, Dr. Cameron, for analysing these papers and continuing to speak out.
Lori
06/11/2015 (8:52 pm)
I am here to tell you that this is very real. I have Chronic Lymes Disease and unfortunately was not diagnosed until many years later. I am well aware that even though my igm levels are still negative, I cannot get rid of the viruses and whatever else is living in me. I cannot get rid of the bacterial infection in the brain that continues to resurface about a aweek or two after antibiotic treatment. I still have nerve damage and lyme arthritis, along with a slew of symptoms that come on without warning, some are fatal, such as chronic and acute pancreatitis, heartmurmur, chronic bronchritis, inflammation of the chest and fluid around the heart, inflammation everywhere for years, chronic EBV that has yet to be put into remissionbsince I was first tested in 2001 when it was 16 times what it should be. It is still extremely high along with Hhv6 that is still very high. I have recurring bouts with the coxsackie virus. This disease effects every organ in your body. I now have a skin disease, vasculitis, polyneuropathy, peripheal nerve disease and so much more. Endocrine issues, gastrotestinal intestinal, blockages, fibroids, lymphadenopathy, and now glaucoma can be noted . I cannot believe that we are made to look like idiots and left to be patronized by all of these who fight against it. I suffer with extreme chronic fatigue and pain. I was on oral antibiotics for 1 year and IV antibiotics starting on 4 years when one day I was rushed to the hospital with CVID and High Cardiac enzymes…I literally was going to die if I did not get off of the antibiotics. So i have been off since last Oct., aside from the chronic sinus infections that stay in my brain which i am assuming causes the fluid pockets in the face and the fluid filled bulbar things on the tip of my nose. Don’t tell me, a person who has been in bed or house bound for a least 6 years that I am a hypochrondriac. This took my job as a high school English teacher, and it took me away from a lot of mom stuff for four. I was a strong, independant person that started very early in the morning and ended very late at night. This started when my youngest was 3 and he is now 171/2. Help us if you can. We have spent well over 100,000 dollars out of pocket. If you know of any clinical trials that is offering some kind of new antibiotic or any treatment that will in your opinion work, please , please help me out. I have a cousin that is in the same medical state that I am in along with her husband and two kids. All of us have had positive Lyme’s test.